Early Predictors of Acute Kidney Injury (AKI) in a Sample of Egyptian Full Term Neonates
Mohamed Abdelaziz El-Gamasy
DOI10.21767/2471-299X.1000054
Mohamed Abdelaziz El-Gamasy*
Tanta University Faculty of Medicine, Tanta, Gharbia Governorate, Egypt
- *Corresponding Author:
- El-Gamasy MA
MD, PhD Pediatrics, Tanta University Faculty of Medicine
Tanta, Gharbia Governorate, Egypt
Tel: +201208136076, +20403333666
E-mail: mgamsy@gmail.com
Received date: September 01, 2017; Accepted date: September 25, 2017; Published date: September 29, 2017
Citation: El-Gamasy MA (2017) Early predictors of Acute Kidney Injury (AKI) in a sample of Egyptian full term Neonates. Med Clin Rev. 3:12. doi: 10.21767/2471-299X.1000054
Abstract
Background: AKI is an independent predictor of morbidity and mortality for critically ill neonates at Neonatal Intensive Care Unit (NICU). Cystatin-C and beta 2 microglobulin are two promising early biomarkers for AKI.
Aim of work: It was to compare between serum creatinine, Cystatin-C and beta 2-microglobulin as early markers for AKI in neonates.
Subjects and methods: This study was carried out on 120 neonatal patients incubated at NICUs of Tanta university hospitals. 60 neonates meeting AKI diagnostic criteria of neonatal Kidney Disease Improving Global Outcome (KDIGO) served as group (1), 60 healthy age and sex matched neonates served as controls (group 2).
Results: At 1st day of incubation, there were significant increase in mean values of Cystatin C and beta 2 microglobulin in patients when compared to controls (2.2 ± 0.5) vs. (0.5 ± 0.2) and (7.2 ± 2.4) vs. (1.9 ± 0.4) respectively while there was no significant difference in that of serum creatinine in both studied groups. At a cut off value ≥ 1.5 (mg/L), beta 2 microglobulin had the highest sensitivity for early prediction of neonates with AKI (98%) with specificity 80%. Cystatin-C at a cut off value ≥ 0.6 (mg/L), had a good sensitivity (85%) with specificity 80%. While serum creatinine had at cut off value ≥ 0.5 (mg/L) the lowest sensitivity (41.5%) with specificity 52.7%.
Conclusions: Serum levels of beta 2 microglobulin and cystatin C were more sensitive and more specific than serum creatinine for early prediction of neonatal AKI in NICU.
Keywords
Cystatin-C; Beta 2-microglobulin; Acute kidney injury; Neonates
Introduction
Neonatal AKI is a common practical disorder faced in NICU. The commonest causes are sepsis, severe respiratory distress (RD) and hypoxic ischemic encephalopathy (HIE) [1]. Early identification of neonatal AKI is very important for planning of different lines of treatment of ill neonates. Early management of neonatal AKI can prevent dangerous complications. In most of NICU, serum creatinine is used for diagnosing AKI which is not ideal as it has tendency toward increase in late phases of AKI at which management could be more aggressive, more costly and less efficient [2-4]. Βeta 2-microglobulin and Cystatin-C (Cys-C) were known as low-molecular weight (LMW) protein structures which were formed at steady ratio by different body cells e.g. nucleated cell. Serum values of beta 2- microglobulin and Cystatin-C had ideal criteria for early diagnosis of AKI as they were freely filtered by the glomerular tuft of capillaries and freely reabsorbed and metabolized by proximal convoluted tubular cells of kidney [5-8]. The objective of the present study was to assess serum Cystatin-C and Beta 2-Microgloulin as early biomarkers for AKI in a sample of Egyptian neonates.
Materials and Methods
Design of the study and setting
This Case Controlled study was conducted after approval from the Ethical Research Committee of the Faculty of Medicine of Tanta University and informed parental written or verbal consents from all subjects involved in the study, upon 60 neonatal patients who were hospitalized at NICUs of Tanta Universality hospital in the period from August 2016 to July 2017. Their gestational ages ranged from 38.4 + 1.2 weeks. They were 33 males and 27 females, the patients were diagnosed as AKI according to diagnostic criteria of Neonatal Kidney Disease Improving Global Outcome (KDIGO) [9] as group (1). Sixty completely healthy neonates of comparable age and sex during their regular neonatal checkup were served as controls (group 2). Their gestational ages ranged from 38.5 + 1.2 weeks. They were 42 males & 18 females.
Inclusion criteria
Neonatal patients with AKI was diagnosed when serum creatinine serially increase > 0.3 mg/dl within 48 hours or serum creatinine > 1.5-1.9 X reference range of serum creatinine (meaning the lowest previous value) within 7 days or urine output from 0.5 to 1 ml/kg/hr for 1st 24 hours of life according to proposed KDIGO definition for neonatal AKI [9].
Exclusion criteria
Neonates with perinatal history of maternal azotemia or kidney disorders, congenital anomalies of kidney or urinary tract and those neonates who died during the research.
Study protocol
All patients and controls were subjected to through history taking (onset of AKI, or other critical illness, need and duration of mechanic ventilation, number of organ system failure and disease outcome), full clinical examination (especially weight and height for age percentiles according to Egyptian growth curves [10].
The routine laboratory tests were: Complete blood count (CBC) by ERMA BC 210, C-Reactive protein (CRP) by Adiva Centaur CP/Immunoassay, Prothrombin time (PT) and activity by Sysmex CA 1500, Serum creatinine by kinetic assay using Kone Lab Prime 60I), some liver function tests (AST & ALT) by Kone Lab Prime 60I), and plasma levels serum Cystatin C and Beta 2-Microglobulin.
Sampling
Samples withdrawn at 1st and 3rd day of admission: Seven milliliters of venous blood was drawn under aseptic conditions and distributed as follows:
(a) One milliliter of whole blood was taken in an EDTA vacutainer (violet cap) and mixed gently. This sample was used to measure complete blood count (CBC) which was done for all samples by sysmex KX-21N.
(b) Three milliliters of blood were taken in citrated test tubes (blue cap), the samples were centrifuged at 1500 rpm for 15 min. The separated plasma was used for the assay of PT, INR and PTT and serum Cystatin C and Beta 2-Microglobulin. Which were measured using human enzyme-linked immunosorbent assay (ELISA) (sandwich technique) kits.
(c) Three milliliters of blood were taken in plain test tubes without anticoagulant (red cap) and left until coagulation. After coagulation, the samples were centrifuged at 1500 rpm for 15 min. The separated serum was used for the assay of ALT&AST and serum creatinine (Cr)], Serum Creatinine was evaluated with the Bio Systems reagent kit provided by Bio Systems S.A. (Barcelona, Spain) by modified Jaffe reaction. Serum urea was determined by the enzymatic colorimetric test, using a Diamond kit, (Diamond Diagnostics, Holliston, USA) and C-reactive protein (CRP), Quantitative C- Reactive protein CRP: serum was separated and analyzed using Turbox plus. Results were considered positive above 6 mg/l.
Test principle for plasma levels of serum Cystatin C
It was measured by Kit used the Bio Vendor human Cystatin C ELISA. We incubate standards, quality controls and patients samples in micro titrate plate wells pre-coated with polyclonal anti-human Cystatin C antibody. Polyclonal anti-human Cystatin C antibody which was conjugated with horseradish peroxidase (HRP) was added to the wells after half hour of incubation and washing, and then incubated for half hour with the captured Cystatin C. After another washing step, the remaining HRP conjugate reacted with the substrate solution (TMB). The reaction resulted in acidic solution with absorbance of the resulting yellow product which measured by spectrophotometry at 450 nm; the absorbance was parallel to the concentration of Cystatin C. A was constructed by plotting the absorbance values against the concentrations of Cystatin C standards and concentrations of the unknown patient samples constructed a standard curve of results.
Test principle for plasma levels of Beta 2- Microglobulin
It was measured by highly purified anti-human-B2M antibodies which were bound to micro wells. HRP conjugate anti-human B2M immunologically detected the bound B2M, forming a conjugate/B2M/antibody complex. Washing of the micro wells removed the unbound conjugates. An enzyme substrate in the presence of bound conjugate hydrolyzed to form a blue color. The addition of an acid finished the reaction, forming a yellow end-product. The intensity of this yellow color was measured photo metrically at 450 nm. The amount of color was directly proportional to the concentration of B2M present in the original samples [11].
Statistical analysis
Data were fed to the computer and analyzed using IBM SPSS software package version 20.0. (Armonk, NY: IBM Corp). Qualitative data were described using number and percent. Quantitative data were described using range (minimum and maximum), mean, standard deviation and median. Significance of the obtained results was judged at the 5% level.
The used tests were: Chi-square test for categorical variables, to compare between different groups. Fisher’s Exact or Monte Carlo correction: Correction for chi-square when more than 20% of the cells have expected count less than 5. Ftest (ANOVA): For normally quantitative variables, to compare between more than two groups, and Post Hoc test (LSD) for pair wise comparisons. Mann Whitney test: For abnormally quantitative variables, to compare between two studied groups. Kruskal Wallis test: For abnormally quantitative variables, to compare between more than two studied groups. Receiver operating characteristic curve (ROC): The area under the ROC curve denotes the diagnostic performance of the test. Area more than 50% gives acceptable performance and area about 100% is the best performance for the test. The ROC curve allows also a comparison of performance between two tests, Kaplan-Meier and cox regression was done for the significant relation with progression free survival and overall survival [12].
Results
Table 1 summarized demographic and laboratory data of the studied groups, there is no statistically significant difference between studied neonates and controls as regard gestational age, sex, mode of delivery, or birth weight but there was statistically significant decrease in studied patients as regard APGAR scoring at 1 min and at 5 min and hematocrit value when compared to controls (p<0.05).
| Controls | Patients | Statistical test | ||||
|---|---|---|---|---|---|---|
| (n=60) | (n=60) | test value | P valu e | |||
| Gestational age (weeks) | Mean ± SD | 38.4 + 1.2 | 38.5 + 1.2 | t=0.3 | 0.77 | |
| Gender | Male : | No (%) | 33 (55) | 42 (70) | X2=0. 16 | 0.69 |
| Fem ale: | No (%) | 27 (45) | 18 (30) | |||
| Mode of delivery | NVD | No (%) | 21 (35%) | 24 (40%) | X2 | 0.9 |
| CS | No (%) | 39 (65%) | 36 (60%) | 0.02 | ||
| Birth weight (Kg) | Mean ± SD | 3.1 + 46.7 | 3.13 + 57.5 | t=1.0 43 | 0.3 | |
| Apgar score | at 1 min | Mean ± SD | 6.2 + 0.8 | 8.4 + 0.8 | t=7.1 | <0.0 01* |
| at 5 min | Mean ± SD | 7.3 + 0.7 | 9.5 ± 0.7 | t= 8.12 | <0.0 01* | |
| Hematocr it (%) | Mean ± SD | 43.4 + 10.6 | 53.8 ± 7.1 | t=5.3 4 | <0.0 01* | |
Table 1: Demographic and laboratory characteristics of the cases and the controls.
Table 2 showed that at first day of incubation, there were statistically significant increase in mean values of Cystatin C and beta2 microglobulin in patients when compared to controls, (2.2 ± 0.5) vs. (0.5 ± 0.2,) and (7.2 ± 2.4) vs. (1.9 ± 0.4) respectively while there was no significant difference in mean value of serum creatinine in patients when compared to controls (0.8 ± 0.1) vs. (0.5± 0.2) mg/dl. In our work, we studied the same renal parameters on 3rd day of incubation, there was highly statistically significance increase in Cystatin C, Beta 2 microglobulin and serum creatinine in patient group when compared to control group.
| Patients | Controls | Student t test | ||||
|---|---|---|---|---|---|---|
| t value | P value | |||||
| Creatinine Range (mg/dl) |
Day 1 | Range | 0.6-0.9 | 0.45-0.8 | 1.34 | 0.13 |
| Mean ± SD | 0.8 ± 0.1 | 0.54 ± 0.2 | ||||
| Days 3 | Range | 1.4–1.6 | 0.4–0.7 | 2.53 | 0.048* | |
| Mean ± SD | 1.5 ± 0.6 | 0.5 ± 0.2 | ||||
| Cys-C (mg/L) | Day 1 | Range | 0.7–3.9 | 0.4–0.7 | 3.26 | 0.01* |
| Mean ± SD | 2.2 ± 0.5 | 0.5 ± 0.2 | ||||
| Days 3 | Range | 1–6.7 | 0.4–0.7 | 7.64 | 0.001* | |
| Mean ± SD | 4.2 ± 1 | 0.5 ± 0.1 | ||||
| B2M (mg/L) | Day 1 | Range | 1.8–15.1 | 1.4–2.5 | 5.34 | 0.002* |
| Mean ± SD | 7.2 ± 2.4 | 1.9 ± 0.4 | ||||
| Days 3 | Range | 3.4–21.7 | 1.4–2.5 | 9.34 | 0.001* | |
| Mean ± SD | 12.5 ± 3.3 | 2 ± 0.3 | ||||
Table 2: Means of serum creatinine, serum cystatin-C (Cys-C) and Beta-2 microglobulin (B2M) and on days 1 and 3 of admission.
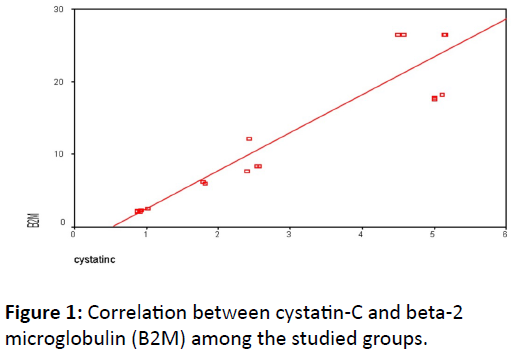
Figure 1 clarified that there was a significant positive correlation between Cystatin
C and Beta2 microglobulin in patients group (p<0.05).
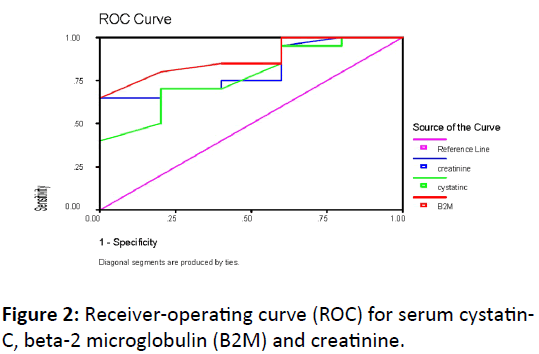
Table 3 and Figure 2 compared Receiver of Characteristics (ROC) curves for validity of plasma levels of Cystatin C and beta-2 microglobulin respectively in early prediction of AKI in neonates.
| Β2M (mg/L) | Cystatin-C ( mg/L) | Serum creatinine(mg/dl) | |
|---|---|---|---|
| Cut-off | 1.5 | 0.6 | 0.5 |
| Sensitivity (%) | 98 | 85 | 41.5 |
| Specificity (%) | 80 | 80 | 52.7 |
| Positive predictive value (PPV) (%) | 84.2 | 83.6 | 66.3 |
| Negative predictive value (NPV) (%) | 77.4 | 76.3 | 70.3 |
| Accuracy (%) | 90.7 | 82.9 | 69.5 |
Table 3: Validity of serum creatinine, cystatin-C and beta-2 microglobulin (B2M) for predicting AKI in the studied neonates.
Serum Beta 2 Microglobulin was more sensitive than serum Cystatin C which was in turn more sensitive than serum creatinine in early prediction of AKI in the studied neonates. At a cut off value ≥ 1.5 (mg/L), beta 2 microglobulin had sensitivity of 98% with specificity 80%, PPV 84.2%, NPV 77.4% and accuracy 90.7% while at a cut off value ≥ 0.6 (mg/L), Cystatin-C had sensitivity of 85% with specificity 80%, PPV 83.6%, NPV 76.3% and accuracy 82.9%. On other side, serum creatinine had at cut off value ≥ 0.5 (mg/L), sensitivity of 41.5%, specificity 52.7%, PPV 66.3%, NPV 70.3% and accuracy 69.5%.
Discussion
AKI is defined as a rapid reversible rise in serum creatinine and nitrogenous wastes levels, in addition failure of the renal glomeruli and tubules to maintain fluid and electrolyte and acid base balance [13,14].
Most of publications reported that single measurement of serum creatinine level was neither sensitive nor specific for reflecting diagnosis or severity of AKI. It cannot distinguish between variable classes of AKI.
Early diagnosis of AKI made patients to receive optimal treatment options at optimal time including adjustment of fluid therapy and other supportive measures and protect the patients from serious complications. All result in improvement of patient outcomes.
Cystatin C and Beta 2 Microglobulin had been considered two of early indicators for predicting AKI in adults, pediatrics and in neonates [15,16].
In this work, we evaluated three of parameters of renal functions including serum creatinine, Serum Cystatin C and Beta 2 Microglobulin in 60 neonates during the first day of incubation to NICU (Day 1) and during the 3rd day of incubation ion (Day 3).
During the first day of incubation, serum Cystatin C increased in studied patients and remained within normal values in healthy controls. Our results were in accordance with Soni SS et al. [17], Nguyen MT et al. [18] and Delanaye P et al. [19] who reported nearly similar results [17-19].
In our study, serum B2M levels increased in studied patients and remained within normal values in healthy controls. Donadio C et al. [20], Filler G et al. [21] and Jovanovic D et al. [22] concluded similar findings.
Sarkar et al. [23] demonstrated that serum creatinine in their research work was a neither sensitive nor reliable biomarker for early identification of mild to moderate degrees of AKI. In addition, several previously published researches including Laterza et al. [24], Le Bricon et al. [25], Bianchi et al. [26] and John et al. [27] had concluded that serum cystatin C and beta2 microglobulin were easily applicable, highly sensitive indicators for AKI in their study when compared to routinely used serum creatinine.
In our study, the results in 3rd day of incubation, both beta 2 microglobulin an cystatin C remained the studied neonates higher than in controls, This observation confirmed more advantages of beta2 microglobulin an cystatin C than routine serum creatinine as early biomarkers for neonatal AKI [12,22,28-34].
Conclusion
Measurements of serum levels of beta 2 microglobulin and cystatin C were more sensitive and more specific than serum creatinine as renal function tests for early prediction of neonatal AKI in NICU.
References
- Schrier RW, Wang W, Poole B, Mitra A (2004) Acute renal failure: Definitions, diagnosis, Pathogenesis and therapy. J Clin Invest 114: 5-14.
- Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, et al. (2007) Acute kidney injury network: Report of an initiative to improve outcomes in acute kidney injury. Crit Care 8: 204-212.
- Rosner MH (2009) Urinary biomarkers for the detection of renal injury. Adv Clin Chem 49: 73-97.
- Rosner MH, Bolton WK (2006) Renal function testing. Am J Kidney Dis 47: 174-183.
- Grubb AO (2000) Cystatin C- Properties and use as diagnostic marker. Adv Clin Chem 35: 63-99.
- Dharnidharka VR, Kwon C, Stevens G (2002) Serum cystatin C is superior to serum creatinine as a marker of kidney function: A meta-analysis. Am J Kidney Dis 40: 221-226.
- Saeidi B, Koralker R, Griffin RL, Halloran B, Ambalavayam N, et al. (2015) Impact of gestational age, sex and postnatal age on urine biomarkers in oreterm neonates. Ped Nephrol 30: 2037-2044.
- Schaub S, Wilkins JA, Antonovici M, Krokhin O, Weiler T, et al. (2005) Proteomic-based identification of cleaved urinary beta2-microglobulin as a potential marker for acute tubular injury in renal allografts. Am J Transplant 5: 729-738.
- Neonatal Kidney Disease Improving Global Outcome (KDIGO): Proposed definition of AKI in Neonates. Kidnry International supplem. Seminars in Fetal & Neonatal Medicine (2016).
- National Center for Health Statistics.
- Le Bricon T, Thervet E, Benlakehal M, Bousquet B, Legendre C, et al. (1999) Changes in plasma cystatin C after renal transplantation and acute rejection in adults. Clin Chem 45: 2243-2249.
- Kirkpatrick LA, Feeney BC (2013) A simple guide to IBM SPSS statistics for version 20.0. Student ed. Belmont, Calif.: Wadsworth, Cengage Learning.
- Andreoli SP (2009) Acute kidney injury in children. Pediatr Nephrol 24: 253-263.
- Moran SM, Myers BD (1985) Course of acute renal failure studied by a model of creatinine kinetics. Kidney Int 27: 928-937.
- Vaidya VS, Ferguson MA, Bonventre JV (2008) Biomarkers of acute kidney injury. Annu Rev Pharmacol Toxicol 48: 463-493.
- Askenazi DJ, Ambalavanan N, Goldstein SL (2009) Acute kidney injury in critically ill newborns: What do we know? What do we need to learn? Pediatr Nephrol 24: 265-274.
- Soni SS, Ronco C, Katz N, Cruz DN (2009) Early diagnosis of acute kidney injury: The promise of novel biomarkers. Blood Purif 28: 165-174.
- Nguyen MT, Devarajan P (2008) Biomarkers for the early detection of acute kidney injury. Pediatr Nephrol 23: 2151-2157.
- Delanaye P, Lambermont B, Chapelle JP, Gielen J, Gerard P, et al. (2004) Plasmatic Cystatin C for the estimation of glomerular filtration rate in intensive care units. Intensive Care Med 30: 980-983.
- Donadio C, Lucchesi A, Ardini M, Giordani R (2001) Cystatin C, beta 2-microglobulin, and retinol binding protein as indicators of glomerular filtration rate: Comparison with plasma creatinine. J Pharm Biomed Anal 24: 835-842.
- Filler G, Priem F, Lepage N, Sinha P, Vollmer I, et al. (2002) Beta-trace protein, cystatin C, beta(2)-microglobulin, and creatinine compared for detecting impaired glomerular filtration rates in children. Clin Chem 48: 729-736.
- Jovanovic D, Krstivojevic P, Obradovic I, Durdevic V, Dukanovic L (2003) Serum cystatin C and beta2-microglobulin as markers of glomerular filtration rate. Ren Fail 25: 123-133.
- Sarkar PD, Rajeshwari G, Shivaprakash TM (2005) Cystatin C-A novel marker of glomerular filtration rate: A review. Indian J Clin Biochem 20: 139-144.
- Laterza OF, Price CP, Scott MG (2002) Cystatin C: An improved estimator of glomerular filtration rate? Clin Chem 48: 699-707.
- Le Bricon T, Leblanc I, Benlakehal M, Gay- Bellile C, Erlich D, et al. (2005) Evaluation of renal function in intensive care: Plasma cystatin C vs. creatinine and derived glomerular filtration rate estimates. Clin Chem Lab Med 43: 953-957.
- Bianchi C, Donadio C, Tramonti G, Consani C, Lorusso P, et al. (2001) Reappraisal of serum beta2-microglobulin as marker of GFR. Ren Fail 23: 419-429.
- John GT, Fleming JJ, Talaulikar GS, Selvakumar R, Thomas PP, et al. (2003) Measurement of renal function in kidney donors using serum cystatin C and beta(2)-microglobulin. Ann Clin Biochem 40: 656-658.
- Christenson A, Ekberg J, Grubb A, Ekberg H, Lindstrom V, et al. (2003) Serum cystatin C is a more sensitive and more accurate marker of glomerular filtration rate than enzymatic measurements of creatinine in renal transplantation. Nephron Physiol 94: 19-27.
- Julier K, da Silva R, Garcia C, Bestmann L, Frascarolo P, et al. (2003) Preconditioning by sevoflurane decreases biochemical markers for myocardial and renal dysfunction in coronary artery bypass graft surgery: A double-blinded, placebo-controlled, multicenter study. Anesthesiology 98: 1315-1327.
- Stevens LA, Levey AS (2005) Measurement of kidney function. Med Clin North Am 89: 457-473.
- Bouvet Y, Bouissou F, Coulais Y, Seronie-Vivien S, Tafani M, et al. (2006) GFR is better estimated by considering both serum cystatin C and creatinine levels. Pediatr Nephrol 21: 1299-1306.
- Mussap M, Dalla Vestra M, Fioretto P, Saller A, Varagnolo M, et al. (2002) Cystatin C is a more sensitive marker than creatinine for the estimation of GFR in type 2 diabetic patients. Kidney Int 61: 1453-1461.
- Newman DJ, Thakkar H, Edwards RG, Wilkie M, White T, et al. (1995) Serum cystatin C measured by automated immunoassay: A more sensitive marker of changes in GFR than serum creatinine. Kidney Int 47: 312-318.
- Harmoinen A, Ylinen E, Ala-Houhala M, Janas M, Kaila M, et al. (2000) Reference intervals for cystatin C in pre- and full-term infants and children. Pediatr Nephrol 15: 105-108.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences