Contributing Factors to Non-Adherence among Chronic Kidney Disease (CKD) Patients: A Systematic Review of Literature
Geldine Chironda and Busisiwe Bhengu
DOI10.21767/2471-299X.1000038
Geldine Chironda1* and Busisiwe Bhengu2
1Rory Meyers College of Nursing, New York University, New York, USA
2College of Medicine and Health Sciences, School of Nursing and Midwifery, University of Rwanda, Kigali, Rwanda
- *Corresponding Author:
- Chironda G
Rory Meyers College of Nursing
New York University, New York, USA
Tel: 0027747037984
E-mail: gerrychironda@yahoo.co.uk
Received date: October 11, 2016; Accepted date: November 07, 2016; Published date: November 14, 2016
Citation: Chironda G, Bhengu B. Contributing Factors to Non-Adherence among Chronic Kidney Disease (CKD) Patients: A Systematic Review of Literature. Med Clin Rev. 2016, 2:29. doi: 10.21767/2471-299X.1000038
Copyright: © 2016 Chironda G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Non-adherence to comprehensive management of Chronic Kidney Disease (CKD) remains a significant barrier to effective management of the population. Interventions to improve adherence need to target the contributing factors to enhance the quality of life.
Objective: To highlight the factors contributing to non-adherence in CKD patients.
Methods: Articles were identified from online data bases namely Medline, PubMed, Cinahl, Google scholar and Grey literature. A comprehensive search was done to identify articles which highlight the factors contributing to non-adherence in CKD patients. The following words were used for this search: Adherence & non-adherence, factors contributing to non-adherence to dialysis, medication, diet and fluid, CKD patients. 96 of them were identified.
Results: Six categories of factors contributing to nonadherence were identified. These were patient related, socioeconomic factors, psychological factors, therapy related factors, pathophysiological related factors and health care system related factors.
Conclusion: Non adherence remains a major obstacle in the effective management of CKD population. There is need for collaborative approach to devise measures that eliminate relevant contributing factors to non-adherence in CKD patients.
Keywords
Chronic Kidney Disease (CDK); Adherence; Non-adherence; Medication; Haemodialysis; Continuous Ambulatory Peritoneal Dialysis (CAPD); Dietary and fluid restriction
Introduction
Patients undergoing treatment for Chronic Kidney Disease (CKD) are required to follow this multifaceted and comprehensive treatment that is complex and difficult to comprehend [1]. Comprehensive management of CKD patients includes dialysis, medication, fluid and dietary restriction [2]. The provision of CKD comprehensive patient care in terms of dialysis plan, medication, fluid and dietary restriction is crucial in slowing the progression and complications of CKD. However, evidence indicated that a substantial proportion of CKD patients were found to deviate from prescribed dialytic, medication, dietary and fluid recommendations [3] causing ongoing challenges in the health care.
Non-adherence rates to dialysis among CKD patients found in previous studies range from 2% to 98% [3-8]. Low rates of adherence to fluid restriction ranging from 9.7% to 72%, have been found in previous studies [9-12]. Similarly, poor adherence to medication and dietary restriction has been documented among CKD patients, ranging from 3% to 80% and 2% to 81% respectively [11,13-15].
Non-adherence to dialysis is a cause for concern as it leads to several life-threatening complications. Tolkof-Rubin [16] emphasises that poor adherence to haemodialysis increases the risk of complications in CKD patients. Complications include chronic anaemia, brain dysfunction, congestive heart failure, decreased function of white blood cells, excessive bleeding, infections, weakness of bones and pulmonary complications.
Mortality rates for individuals with CKD remain high because of nonadherence and without adequate dialysis, death occurs from build-up of fluids and waste products in the body [17]. According to the 2010 Global Burden of Disease Study, CKD ranked 27th in the list of causes of total number of global deaths in 1990, with age standardised annual death rate of 15.7 per 100,000, but rose to 18th in 2010, with annual death rate of 16.3 per 100,000 [18].
Non-adherence to CAPD is the leading cause of peritonitis in CKD patients. Peritonitis remains a significant problem in peritoneal dialysis and contributes to mortality. In India, Mawar et al. [19] did an observational study to find the prevalence of noncompliance to the CAPD procedure and its influence on the incidence of peritonitis. Peritonitis occurred in 60% of non-adherence patients and fully compliant patients had no peritonitis.
These findings indicate that poor compliance in performing CAPD procedure is a modifiable risk factor for peritonitis. Other complications of non-adherence to CAPD include pulmonary oedema, hypertension, hospital readmissions and septicaemia. In addition, poor adherence to dialysis has been reported as the most common cause of failure to respond to medication and of additional and unnecessary tests, dosage adjustment, changes in treatment plans, emergency department visits and hospitalisations, which ultimately increase the costs of medical care [20].
Consequences of excessive fluid intake and associated chronic fluid overload include treatment-related fatigue and dizziness, lower-extremity oedema, ascites, left ventricular hypertrophy and congestive heart failure, hypertension, shortness of breath, and pulmonary vascular congestion or acute pulmonary oedema [8,21,22]. Excessive fluid overload contributes to increased morbidity [8,23] and high mortality [8,21] in CKD patients.
In a study of more than 3000 patients with CKD, medication non-adherence has been associated with uncontrolled hypertension, which is associated with increased risk of CKD stage 5, and intensified blood pressure control may slow progression of CKD [20]. Inability to adhere with dietary restriction results in a faster progression of kidney disease into kidney failure and the need for transplant. Observational data from epidemiologic studies provide evidence that dietary protein intake is related to the progression of renal disease [24].
Non-adherence to dietary and medication regimes can result in chronically elevated serum levels of phosphate, which play an important role in the development of secondary hyperparathyroidism and renal osteodystrophy. Further, elevated levels of phosphate may increase coronary artery disease even in young patients, leading to significantly increased risk for mortality. Elevated blood phosphorus concentrations are associated with increased mortality in ESRD patients [25] and increase the risk for cardiovascular events, at least in part by contributing to vascular calcification [26]. Cozzolino et al. [26] show that mortality risk increases when the serum phosphorus levels chronically exceed 6.5 mg/dl as a result of nonadherence to dialysis and diet restriction.
Non-adherence carries a huge economic burden and yearly expenditure for the consequences of non-adherence has been estimated to be in the hundreds of billions of US dollars [27]. Estimation of hospitalisation costs due to medication nonadherence is as high as 13.35 billion dollars annually in the United States alone. It is clear that non-adherence results in a combination of wasted medical care dollars, wasted time and energy for patients and health care providers as well as frustration and dissatisfaction all the parties involved [28].
The Australian Institute of Health and Welfare estimated that the total expenditure on kidney failure disease in 2001 was 647 million dollars and the corresponding figure for the UK National Health Service in 2010 was 1.45 billion pounds, which is about 1.3% of all heath spending [29]. These figures are for adhering patients; for non-adherent cases, the cost of care will be three times the normal spending on the kidney failure population. Thus it is clear that non-adherence often results in wasted medical-care dollars [27,30].
The detrimental effects of non-adherence with dialysis, medication, fluid and dietary restriction need serious consideration as these impacts on the quality of life of CKD patients. Therefore, in order to formulate effective strategies that combat non-adherence in CKD patients, there is a need to systematically review the contributing factors in all four modalities since this is a comprehensive treatment. An understanding of these contributing factors will therefore inform the overall planning of CDK management. Despite the evidence that indicates factors contributing to non-adherence in dialysis, medication, dietary and fluid restriction in CKD population, there are no summative reviews on these factors in all four management modalities.
Purpose of the Review
The purpose of the review is to highlight the contributing factors to non-adherence among CKD patients.
Methodology
Articles from 1993–2015 were identified from online data bases namely Medline, PubMed, Ebsco Host, CINAHL, google scholar and grey literature. A comprehensive search was done to identify studies that identify and explore the factors contributing to nonadherence in CKD.
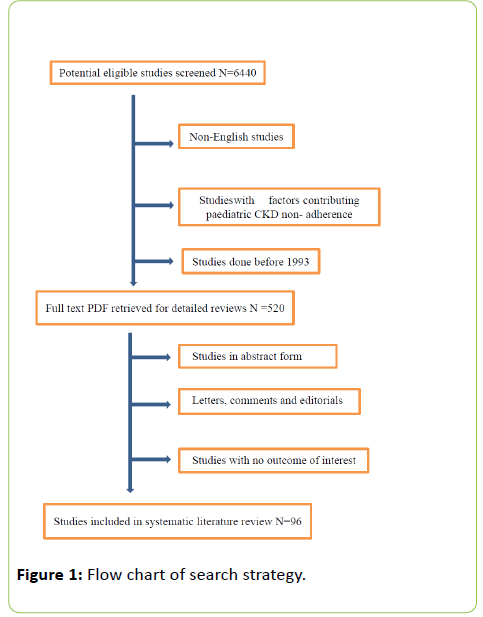
The following words were used for this search: Adherence & non-adherence, factors contributing to non-adherence to dialysis, medication, diet and fluid, consequences of non-adherence in CKD patients. The review included articles written in English only as there were some which covered non- English speaking countries. Qualitative and quantitative studies were included as the review used studies that identifies and explore factors contributing to non-adherence in CKD population. Excluded were studies with factors contributing to non-adherence in comments, editorials and studies with no outcome of interest were excluded from the systematic review (Figure 1) shows the search strategy.
Results
Six categories of factors contributing to non-adherence in CKD patients were identified. They include socio-economic factors, therapy-related factors, patient-related factors, psychological factors, disease-related factors and health care system-related factors. Table 1 reveals the categories of factors contributing to non-adherence in CKD patients.
| Identified categories of factors contributing to non-adherence in CKD patients |
|---|
| Patient related factors Socioeconomic factors Psychological factors Health care related factors Therapy related factors Disease related factors |
Table 1: Categories of factors contributing to non-adherence in CKD patients.
Discussion of Results
Six categories of factors contributing to non-adherence in CKD patients are patient related, psychological, disease related, socioeconomic, therapy related and health care system related factors. There are different sub factors for each category which contributes to non-adherence as shown in Table 2.
| Categories of factors contributing to non-adherence | Sub factors for each category |
|---|---|
| Patient related factors | Age Gender Level of education Health beliefs Interpersonal communication |
| Socioeconomic status | Income status Employment status Social support of families Peer support |
| Psychological factors | Depression Stress Irrational thoughts Perceived physical health Disturbance in self-concept |
| Health care related factors | Availability of dialysis centres Accessibility of dialysis centres Strict selection criteria Economic resources |
| Therapy related factors | Muscle cramps Intra dialytic Hypotension Chest pain Physical fatigue |
| Disease related factors |
Gastrointestinal problems Uraemia |
Table 2: Categories and specific factors contributing to nonadherence in CKD patients.
Patient-Related Factors
Patient-related factors appear to affect adherence of CKD patients. Age has been found to be a determinant in adherence issues. Younger patients and those diagnosed as having chronic illnesses are less adherent. Higher adherence behaviour is found in older patients [9,10,20,31]. Kutner et al. [7] reported similarly that young age is associated with nonadherence in the CKD population. In addition, being male is consistently associated with non-adherence [9,10]
Level of education has also been cited as a determinant in adherence behaviour in chronic illnesses such as CKD. Low education has been found to cause decreased adherence due to poor correlation with knowledge of disease and treatment [32]. Knowledge appeared to be the chief facilitator of positive adherence to fluid restriction, with accurate self-assessment, positive psychological factors and supportive social contacts are also playing a role [33]. Low health literacy has been reported in dialysis patients and this factor, combined with regimen complexity, may contribute to non-adherence [10,34]. Those with low levels of health literacy find it difficult to follow instructions on how to care for themselves or to adhere to treatment regimens such as taking their medicines [35].
In addition, low health literacy is associated with more hospitalisations, greater use of emergency care, less adherence to treatment recommendations, worse health status, and higher mortality rates [36]. People with good basic literacy and numeracy skills, on the other hand, may struggle to understand and interpret health information in a way that prompts them to act appropriately to protect or enhance their health [37].
Health belief and culture influence how a patient adapts to treatment requirements and have been found to influence phosphate binder adherence in six of nine studies that evaluated health beliefs [38]. In a Chinese population, perceived barriers showed associations with compliance measures, implying that patients who perceived fewer barriers in following the dietary restrictions showed better compliance [39]. Studies have repeatedly shown that forgetting to take medications is a major contributor to non- adherence [40,41].
The interpersonal dynamics of health care and the patient play an important role in determining a variety of patient outcomes including patient adherence to their treatment recommendations. Patients who feel that their physicians communicate well and actively encourage them to be involved in their own care tend to be more motivated to adhere [42-44]. Empathetic communication, involving a thorough understanding of patient’s perspective, improves adherence. Patients who are informed and effectively motivated are also more likely to adhere to their treatment recommendations [45].
Socio-economic Factors
Employment status and income have been investigated in relation to socio-economic status among the CKD population. Low socio-economic status has been reported among CKD patients by Magacho et al. [14], Chironda et al. [4] and Assounga et al. [46] and where the majority of the CKD patients were unemployed. Poverty increases the risk of disorders that predispose CKD to progress and worsens outcomes in those who already have CKD. Prosperity increases access to renal replacement therapy. People in the lowest socio-economic quartile are at a 60% greater risk of CKD than those who are in the highest quartile [47].
The ability of CKD patients to work and lead a productive life is hampered by CKD as they no longer work and are unable to provide for their families [48,49]. Kaitelidou et al. [49] have reported similar findings and highlight unemployment due to CKD as a significant stressor for CKD patients. In their study, more than half of patients receiving dialysis were not able to maintain their profession and some had to retire after the beginning of dialysis. Furthermore, consistent associations with non-adherence were identified for being unemployed [10,50,51].
Admittedly dialysis is an expensive treatment, ranging from 30,000 US dollars to 60,000 US dollars annually in developed countries and from 6000 US dollars to 40,000 US dollars in developing nations [52]. Cost has been implicated in non-adherence in several studies of dialysis patients [4,53]. Most patients in developing countries have no access to health insurance and this makes care for CKD unaffordable and consequently affects their adherence rates to prescribed treatment regimen. According to World Kidney Day [54], the majority of patients commencing dialysis in low income countries die or stop treatment within three months of initiating dialysis due to cost constraints. Limited economic resources of patients in developing countries results in reduced frequency of dialysis and eventually discontinuation of therapy [55].
In addition to a debilitating and disruptive chronic illness, the treatment regimen is complex and demanding, which also this affects personal and social life [56]. Social support of friends, family and renal health professionals as well as family dynamics have been found to influence medication adherence among kidney failure patients [38,57]. Emotionally or genetically related family members of patients can have significant influence on the patient’s engagement in their own care [58]. Excellence in care requires more than just the best care in diagnosis and treatment; it also requires care that addresses every aspect of a patient’s experience. CKD and its treatments can restrict daily activities, employment, family life, and social relationships. This can lead to feelings of isolation. Feeling socially isolated can be stressful and anxiety provoking. Social support has been shown to improve survival and quality of life in dialysis patients [59].
Living with a chronic illness requires emotional support to help make the changes needed to cope and adapt. Peer support is reported to be beneficial to patients with kidney disease and in long-term dialysis therapy [60,61]. Research shows that people often cope better when they interact with peers with whom they identify and share common experiences [62]. In this way, feelings are validated, social isolation and stigma are reduced, hope for the future and optimism grows, and experiences are normalised. Peer mentoring has been shown to be highly effective in helping CKD patients adjust to dialysis and approach end-of-life planning [60,61]. It also improves depression, social isolation, self-esteem, and self-management and consequently better adherence, health and survival.
Psychological Factors
The rate of psychiatric disorders in a population of CKD patients is considerably higher than in any other population with other chronic illnesses [63]. Depression is the most common psychological problem in CKD patients and is associated with both mortality and morbidity [64]. Biochemical imbalance, physiological changes, neurological disturbances, cognitive impairment are additional stressors which contribute to depression in CKD patients [65].
According to Leung [66], diagnosis of CKD creates a turmoil that reaches into all aspects of the patient’s life and precipitates emotions, fear, anger and despair. Consequently, life with CKD becomes challenging, forcing the patient to confront it in a very personal way. Numerous psychosocial stressors affect CKD patients and their families, and their response to such stressors impact negatively on adjustment and response to treatment regimen. Smith et al. [33] cite psychological factors as the most common barriers to fluid restriction, predominantly involving lack of motivation.
Chilcot et al. [67] reported that 20–30% of CKD patients have significant depressive symptoms compared to lifetime prevalence of depression of approximately 16% in the general population. Depressed patients are found to be three times more likely to be non-adherent with treatment recommendations than non-depressed patients [68]. Kimmel et al. [63] investigated the impact of psychosocial factors on behavioural compliance and survival in urban haemodialysis patients and depression was related to decreased adherence to treatment regimen.
In a study which employed a descriptive cross-sectional design to examine the relationship between depressive symptoms and adherence to fluid and dietary restrictions in patients with CKD, common depressive symptoms were identified that were contributing to non-adherence to fluid and dietary intake in the study population [69].
Irrational thoughts such as mental shortcuts (ignoring some medical conditions), altered risk perceptions of behaviours, cognitive trickery (distorted views about controlling conditions) and using denial as form of coping have also been reported to contribute to non-adherence [70]. The challenges associated with living with CKD are significant and may contribute to patients feeling that they have lost control of their lives [71]. Disturbance in self-concept may lead to depression, with associated suicidal thoughts and poor self-esteem manifested by poor self-hygiene, excessive dependency and lack of adherence to treatment requirements [65]. Perceived physical health has also been reported to cause reduced adherence to treatment regimen among CKD patients [4]. Elsevier [72] states that patient’s beliefs about their physical health are important because they influence adherence and adjustment to dialysis.
Health Care System-related Factors
Availability and accessibility of dialysis centres affect adherence to prescribed treatment regimen among CKD patients. The lack of health care resources in low and middle income countries makes renal replacement therapy unavailable, with consequently low adherence to this therapy [73]. In the United States, patients with kidney failure have access to life-saving dialysis treatments paid for by Medicare, while in less affluent countries like South Africa, medical professionals rely on rationing dialysis services [74]. Public hospitals in South Africa strictly limit the number of patients for dialysis to save money for other pressing health priorities [46].
This situation is similar to that of the United States and other developed nations in the 1960s when dialysis first became available. Demand for the procedure was far greater than the supply, and hospital-based committees quietly rationed dialysis much as they do in South Africa and other African countries. In Nigeria, the majority of patients live far from existing dialysis centres and have to travel long distances to receive dialysis, resulting in dialysis inadequacy and frequent disruption of work that leads to job losses and consequent non-engagement with treatment regimen. Problems of transport are one of the most common reasons for absence or late appearance at the scheduled time for dialysis sessions [75].
Therapy-related Factors
Side-effects of haemodialysis are therapy-related factors that affect adherence of CKD patients to the procedure. These include muscle cramps, hypotension and chest pain. Lynch et al. [76], Fidan et al. [77] and Figueiredo et al. [78] all note that muscle cramps are very common and lead to non-adherence to haemodialysis treatment. Muscle cramps is a well-known and distressing adverse effect that may arise during a haemodialysis session, closely related to the volume of ultrafiltration needed, which can reach an occurrence of 10−20% [79].
Muscle cramps associated with haemodialysis can be debilitating and often affect the patient’s adherence with the haemodialysis treatment. Previous studies have reported that 17.9% of patients had early sign-offs of haemodialysis treatment because of muscle cramps [80]. These cramps frequently occur towards the end of the dialysis sessions, sometimes precede hypotension, and are associated with higher fluid removal during HD. Recurrent muscle cramps frequently lead to non-compliance with the prescribed haemodialysis treatment [80] and impact patients’ quality of life [77]. Intradialytic hypotension is a major common complication which has been reported to occur in 16–30% of dialysis sessions [81-83]. Intradialytic hypotension is defined as a fall in systolic or mean arterial pressure of 20 mmHg or greater, in combination with clinical symptoms requiring intervention [82]. Such hypotension event will occur if the rate of fluid removal in the dialyzer exceeds the plasma refilling rate in the patient [84]. In addition, repeated episodes of intradialytic hypotension may cause cardiac fibrosis and cerebral ischemia leading to development of lacunar infarcts [82]. A higher rate of fluid removal is associated with an increased risk of both intradialytic hypotension and mortality [85]. According to the same authors, the safe rate of fluid removal at dialysis should be less than 10 mL/h/kg dry body weight.
Pain is a major health problem in CKD, affecting half of the dialysis patients, and most experience moderate to severe degree of pain [81]. Nevertheless, the impact of chronic pain and its consequences are often underestimated [86]. Again, being on treatment for a longer period of time [10] is associated with non-adherence among CKD patients.
Physical fatigue is one frequently experienced problem among CKD patients on haemodialysis, with approximately 90% of CKD patients reporting lack of energy and feeling tired. Harilall [87] did a study in KZN where CKD patients on dialysis were found to experience physical symptoms such as tiredness, lack of energy, nausea and cramps post dialysis and these were causing limitations in activities of daily living. People with CKD report a reduced capacity to engage in regular activity [88] and difficulties with being able to undertake routine living activities [4]. Athienites et al. [89] found that 25–30% of peritoneal dialysis and haemodialysis patients had mild-tomoderate physical and cognitive impairment due to comorbidity.
Disease-related Factors
Herselman [90] indicates that attempts to convince patients to actively participate in diet and medical regimens do not produce desired outcomes because it is difficult to manage. Previous studies have implicated gastrointestinal complaints as a major contributor to problems of decreased intake and malnutrition [47,91] and suggest that addressing GI issues in patients with renal failure may improve nutritional status [91]. Furthermore, patients with CKD have increased serum leptin and elevated serum acute phase mediators. These mediators decrease oral intake of food. Again, the presence of uremia is a more obvious factor that adds to decreased appetite and nutrient intake [92] contributing to non-adherence. Moreover, CKD patients regard renal diet as tasteless and are continually tempted to continue eating non-renal diet like the rest of the family, as Gordon [91] have noted.
Conclusion
The provision of CKD comprehensive patient care in terms of dialysis plan, medication, fluid and dietary restriction is crucial in slowing the progression and complications of CKD. Non-adherence to comprehensive treatment is a cause for concern as it leads to several life-threatening complications. Excellence in care of CKD patients requires more than just the best care in diagnosis and treatment. It also requires the identification of factors that contribute to non-adherence as this is the cornerstone for management of CKD. Therefore, there is need to formulate effective strategies that combat factors contributing to non-adherence in CKD patients.
Funding
This project received financial support from the College of Health Sciences, School of Nursing and Public Health of the University of KwaZulu-Natal; Durban, South Africa The article was part of literature review done for PHD thesis towards the development of a framework for engagement of CKD patients with their integrated management to improve nephrology care.
Competing Interest
Geldine Chironda and Busisiwe Bhengu declare that there is no financial or personal interest or belief that could affect our objectivity. No potential conflicts of interest exist.
Author Contribution
All authors have contributed to development and writing of the manuscript.
References
- Kaveh K, Kimmel PL (2001) Compliance in haemodialysis patients: multidimensional measures in search of a gold standard. Am J Kidney Dis 37: 244-266.
- Short CD (2012) Principles of Renal Replacement Therapy (RTT). Imaging Technol Urol.
- Griva K, Lai AY, Lim HA, Zhenli Yu Z, Foo MYY, et al. (2014). Nonadherence in Patients on Peritoneal Dialysis: A Systematic Review. Plos ONE 9: e89001.
- Chironda G, Manwere A, Nyamakura R, Chipfuwa T, Bhengu B (2014) Perceived health status and adherence to haemodialysis by End Stage Renal Disease (ESRD) patients: A case of a central Hospital in Zimbabwe. IOSR Journal of Nursing and Health Sciences 22: 31
- Taskapan H, Ates F, Kaya B, Emul M, Kaya M, et al. (2005) Psychiatric disorders and large intradialytic weight gain in patients on chronic haemodialysis. Nephrology 10: 15-20.
- Hecking E, Bragg-Gresham JL, Rayner HC, Pisoni RL, Andreucci VE, et al. (2004) Haemodialysis prescription, adherence and nutritional indicators in five European countries: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dialysis Transplant 19: 100- 107.
- Kutner NG, Zhang R, McClellan WM, Cole SA (2002) Psychosocial predictors of non-compliance in haemodialysis and peritoneal dialysis patients. Nephrol Dialysis Transplant 17: 93-99.
- Leggat JE, Orzol SM, Hulbert-Shearon TE, Golper TA, Jones CA, et al. (1998) Noncompliance in haemodialysis: predictors and survival analysis. Am J Kidney Dis 32: 139-145
- Chan YM, Zalilah MS, Hii SZ (2012) Determinants of compliance behaviours.
- Lam LW, Twinn SF, Chan SWC (2010) Self-reported adherence to a therapeutic regimen among patients undergoing continuous ambulatory peritoneal dialysis. J Adv Nurs 66: 763-773.
- Rambod M, Peyravi H, Shokrpour N, Sareban MT (2010) Dietary and fluid adherence in Iranian haemodialysis patients. The Health Care Manager 29: 359- 364
- Denhaerynck K, Manhaeve D, Dobbels F, Garzoni D, Nolte C, et al. (2007) Prevalence and consequences of nonadherence to haemodialysis regimens. Am J Crit Care 16: 222-235.
- Theofilou P (2012) The effect of sociodemographic features and beliefs about medicines on adherence to chronic kidney disease treatment. J Clin Res Bioethics 3: 1-5
- Magacho EJC, Ribeiro LC, Chaoubah A, Bastos MG (2011) Adherence to drug therapy in kidney disease. Braz J Med Biol Res 44: 258-262.
- Schmid H, Hartmann B, Schiffl H (2009) Adherence to prescribed oral medication in adult patients undergoing chronic haemodialysis: a critical review of the literature. Eur J Med Res 14: 185-190.
- Tolkof-Rubin N (2008) Treatment of irreversible renal failure. Service of the US national library and the national institute. Transplantation 22: 845-850.
- Richard CJ (2006) Self-care management in adults undergoing haemodialysis. Nephrol Nurs J 33: 387.
- Lozano R, Naghavi M, Foreman K (2012) Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380: 2095-128.
- Mawar S, Gupta S, Mahajan S (2012) Non-compliance to the continuous ambulatory peritoneal dialysis procedure increases the risk of peritonitis. Int Urol Nephrol 44: 1243-1249.
- Muntner P, Judd SE, Krousel-Wood M, McClellan WM, Safford MM (2010) Low medication adherence and hypertension control among adults with CKD: data from the REGARDS (Reasons for Geographic and Racial Differences in Stroke) Study. Am J Kidney Dis 56: 447-457.
- Lindberg M, Prutz KG, Lindberg P, Wikström B (2009) Intradialytic weight gain and ultrafiltration rate in haemodialysis: lessons about fluid adherence from a national registry of clinical practice. Haemodialysis Int 13: 181-188.
- Charra B (2007) Fluid balance, dry weight, and blood pressure in dialysis. Haemodialysis International 11: 21-31.
- Holmberg B, Stegmayr BG (2009) Cardiovascular conditions in haemodialysis patients may be worsened by extensive intradialytic weight gain. Haemodialysis International 13: 27-31.
- Lentine K, Wrone EM (2004) New insights into protein intake and progression of renal disease. Curr Opin Nephrol Hypertens 13: 333-336
- Ritz E (2005) The clinical management of hyperphosphatemia. J Nephrol 18: 221.
- Cozzolino M, Brancaccio D, Gallieni M, Slatopolsky E (2005) Pathogenesis of vascular calcification in chronic kidney disease. Kidney Int 68: 429-436.
- DiMatteo MR (2004a) Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Medical Care 42: 200-209.
- DiMatteo MR (2004b) Evidence-based strategies to foster adherence and improve patient outcomes: the author's recent meta-analysis indicates that patients do not follow treatment recommendations unless they know what to do, are committed to doing it, and have the resources to be able to adhere. JAAPA 17: 8-22.
- Kerr M, Bray B, Medcalf J, O'Donoghue DJ, Matthews B (2012) Estimating the financial cost of chronic kidney disease to the NHS in England. Nephrol Dialysis Transplant.
- Rizzo JA, Simons WR (1997). Variations in compliance among hypertensive patients by drug class: implications for health care costs. Clin Ther 19: 1446-1457.
- Hibbard JH, Cunningham PJ (2012) How Engaged Are Consumers in Their Health and Health Care, and Why Does It Matter? Centre for Studying Health System Change 8: 1-9.
- Mitch WE (2007) Chronic kidney disease. Cecil Medicine (23rd edn.) Philadelphia, Pa: Saunders Elsevier.
- Smith K, Coston M, Glock K, Elasy TA, Wallston KA, et al. (2010) Patient perspectives on fluid management in chronic haemodialysis. J Renal Nutri 20: 334-341.
- Browne T, Merighi JR (2010) Barriers to adult haemodialysis patients' selfmanagement of oral medications. Am J Kidney Dis 56: 547-557.
- James JA (2013) Patient Engagement: People Actively Involved in Their Health and Health Care Tend to Have Better Outcomes–and, Some Evidence Suggests, Lower Costs. Project HOPE.
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K (2011) Low health literacy and health outcomes: an updated systematic review. Ann Int Med 155: 97-107.
- Coulter A (2012) Patient engagement—what works? J Ambulatory Care Manag 35: 80-89.
- Karamanidou C, Clatworthy J, Weinman J, Horne R (2008) A systematic review of the prevalence and determinants of nonadherence to phosphate binding medication in patients with end-stage renal disease. BMC Nephrol 9: 2.
- Lee SH, Molassiotis A (2002) Dietary and fluid compliance in Chinese haemodialysis patients. Int J Nurs Stud 39: 695-704.
- Brekke HK, Sunesson Å, Axelsen M, Lenner RA (2004) Attitudes and barriers to dietary advice aimed at reducing risk of type 2 diabetes in first degree relatives of patients with type 2 diabetes. J Hum Nutr Dietetics 17: 513-521
- Shemesh E, Shneider BL, Savitzky JK, Arnott L, Gondolesi GE, et al. (2004) Medication adherence in paediatric and adolescent liver transplant recipients. Paediatrics 113: 825-832.
- Martin KA, Sinden AR (2001) Who will stay and who will go? A review of older adults' adherence to randomized controlled trials of exercise. J Aging Phys Act 9: 91-114.
- Frankel RM (1995) Emotion and the physician-patient relationship. Motivation and Emotion 19: 163-173.
- Saran R, Bragg-Gresham JL, Rayner HC, Goodkin DA, Keen M, et al. (2003) Nonadherence in haemodialysis: associations with mortality, hospitalization, and practice patterns in the DOPPS. Kidney Int 64: 254-262.
- Squier RW (1990) A model of empathic understanding and adherence to treatment regimens in practitioner-patient relationships. Social Science & Medicine 30: 325-339.
- Assounga A, Hariparshad S, Madala N (2012) Kidney Diseases in an African setting. Reach Publishers.
- Vivekanand JHA, Guillermo G, Kunitoshi I, Zou l, Saraladev N (2013) Chronic kidney disease; Global dimension and perspectives. The Lancet Publication.
- Harilall B, Kasiram M (2011) Exploring the bio-psychosocial effects of renal replacement therapy amongst patients in a state hospital in South Africa. Health SA Gesondheid 1: 6.
- Kaitelidou D, Liaropoulos L, Siskou O, Mamas T, Zirogiannis P, et al. (2007) The social and economic consequences of dialysis in patients' lives with chronic renal insufficiency. Nursing 46: 246-255.
- Chan MF, Wong FKY, Chow SKY (2009) Investigating the health profile of patients with end-stage renal failure receiving peritoneal dialysis: a cluster analysis. J Clini Nurs 19: 649-657.
- Yu ZL, Yeoh LY, Seow YY, Luo XC, Griva K (2012) Evaluation of adherence and depression among patients on peritoneal dialysis. Singapore Med J 53: 474- 480.
- Dirks JH, Levin NW (2006) Dialysis rationing in South Africa: a global message. Kidney Int 70: 982-984.
- Alebiosu CO, Ayodele OE (2005) The global burden of chronic kidney disease and the way forward. Ethnicity and Dis 15: 418.
- World Kidney Day (2012) ISN-Global Operations Centre.
- Schieppati A, Perico N, Remuzzi G (2003) Preventing end stage renal disease: the potential impact of screening and intervention in developing countries. Nephrol Dialysis Transplant18: 858-859.
- Morris PL, Jones B (1989) Life satisfaction across treatment methods for patients with end-stage renal failure. The Med J Aust 150: 428- 432.
- Clarke AL, Young HM, Hull KL, Hudson N, Burton JO, et al. (2015). Motivations and barriers to exercise in chronic kidney disease: a qualitative study. Nephrol Dialysis Transplant 30: 1885-1892.
- Purves CS (2015) Patient’s experience with home haemodialysis: a qualitative study. University of Ontario Institute of Technology.
- Thong MS, Kaptein AA, Krediet RT, Boeschoten EW, Dekker FW (2007) Social support predicts survival in dialysis patients. Nephrol Dialysis Transplant 22: 845-850.
- Hughes J, Wood E, Smith G (2009) Exploring kidney patients’ experiences of receiving individual peer support. Health Expectations 12: 396-406.
- Perry E, Swartz J, Brown S, Smith D, Kelly G, et al. (2005) Peer mentoring: a culturally sensitive approach to end-of-life planning for long-term dialysis patients. Am J Kidney Dis 46: 111-119.
- National Kidney Foundation (2009) K/DOQI clinical practice guidelines for chronic kidney disease. Evaluation, classification, and stratification. Am J Kidney Dis 39.
- Kimmel PL, Thamer M, Richard CM, Ray NF (1998) Psychiatric illness in patients with end-stage renal disease. Am J Med 105: 214-221.
- Troidle L, Watnick S, Wuerth DB, Gorban-Brennan N, Kliger AS, et al. (2003) Depression and its association with peritonitis in long-term peritoneal dialysis patients. Am J Kidney Dis 42: 350-354.
- Zalai D, Szeifert L, Novak M (2012) Psychological distress and Depression in patients with chronic kidney disease. In Seminars in dialysis 4: 428- 438.
- Leung DK (2003) Psychosocial aspects in renal patients. Peritoneal Dialysis International 23: S90-S94.
- Chilcot J, Wellsted D, Davenport A, Farrington K (2011) Illness representations and concurrent depression symptoms in haemodialysis patients. J Health Psychol 16: 1127-1137.
- DiMatteo MR, Lepper HS, Croghan TW (2000) Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Int Med160: 2101- 2107.
- Khalil AA, Frazier SK, Lennie TA, Sawaya BP (2011) Depressive Symptoms and Dietary Adherence in Patients with End Stage Renal Disease. J Renal Care 37: 30-39.
- Williams ME (2009) Management of diabetes in dialysis patients. Curr Diabetes Rep 9: 466-472.
- Schatell D, Witten B (2005) Dialysis patient empowerment: what, why, and how. Nephrolog News & Issues 19: 37.
- Elsevier BV (2009) Haemodialysis patient’s beliefs about renal failure and its treatment, patient counselling and education. Am J Med 53: 189-196.
- Fink JC (2010) Chronic kidney disease: the effect of CKD therapies on serum potassium levels. Nature R Nephrol 6: 633-634.
- Odutola TA, Ositelu SB, D'Almeida EA, Mabadeje AF (1989) Five years’ experience of haemodialysis at the Lagos University Teaching Hospital--November 1981 to November 1986. Afr J med med sci 18: 193-201.
- Sayed M, Abdelatty M, ELRawy B, Yasser M, Salman H, et al. (2014). Assessment of socio-economic burden of haemodialysis on ESRD patients in Suez canal cities & Elarish. Am J Res Comm 2 : 7.
- Lynch PG, Abate M, Suh H, Wadhwa NK (2014) Magnesium and Muscle Cramps in End Stage Renal Disease Patients on Chronic Haemodialysis. Adv Nephrol.
- Fidan FBM, Alkan BM, Tousun A, Altunoglu A, Ardicoglu O (2013) Quality of life and correlation with musculoskeletal problems, hand disability and depression in patients with haemodialysis. Int J Rheum Dis.
- Figueiredo AE, Goodlad C, Clemenger M, Haddoub SS, McGrory J, et al. (2012). Evaluation of physical symptoms in patients on peritoneal dialysis. Int J nephrol.
- Meira FS, Figueiredo AE, Zemiarcki J, Pacheco J, Poli-de-Figueiredo E, et al. (2010) Two variable sodium profiles and adverse effects during haemodialysis: a randomized crossover study. Ther Apheresis Dialysis 14: 328-333.
- Rocco MV, Burkart JM (1993) Prevalence of missed treatments and early sign-offs in haemodialysis patients. J Am Soc Nephrol 5: 1178-1183.
- Prabhakar, Singh RG, Singh S, Rathore SS, Choudhary TA (2015) Spectrum of intradialytic complications during haemodialysis and its management: A singlecentre experience. Saudi J Kidney Dis Transpl 26: 168-72.
- Davenport A (2009) The clinical application of CRRT—Current status: Continuous Renal Replacement Therapies in Patients with Acute Neurological Injury. 22: 165-168.
- Yung J (2008) Optimal ultrafiltration profiling in haemodialysis. Nephrol Nurs J 35: 287.
- Palmer BF (2009) Opinion: Can Chronic Volume Overload Be Recognized and Prevented in Haemodialysis Patients? In Seminars in dialysis 22: 489- 491.
- Santoro D, Satta E, Bellinghieri G (2014) Sexual Dysfunction in Chronic Kidney Disease. In Management of Chronic Kidney Disease 319-327.
- Horigan AE, Schneider SM, Docherty S, Barroso J (2013) The experience and self-management of fatigue in haemodialysis patients. Nephrol Nurs J Am Nephrol Nurses' Ass 40: 113.
- Harilall B (2010) Experiences of patients on haemodialysis and continuous ambulatory peritoneal dialysis in end stage renal disease: an exploratory study at a tertiary hospital in KwaZulu-Natal (Doctoral dissertation). University of KwaZuluNatal.
- Tawney KW, Tawney PJ, Kovach J (2003) Renal Research Institute Symposium: Disablement and Rehabilitation in End Stage Renal Disease. Urol Nephrol 16: 447-452.
- Athienites NV, Miskulin DC, Fernandez G, Bunnapradist S, Simon G, et al. (2000) Comorbidity assessment in haemodialysis and peritoneal dialysis using the index of coexistent disease. Semi Dial 13: 320-326.
- Herselman M (2008) Non-adherence to dietary prescriptions in chronic kidney disease: editorial. S Afr J Clin Nutr 21: 13-14.
- Gordon EJ, Prohaska TR, Gallant M, Siminoff LA (2009) Self-care strategies and barriers among kidney transplant recipients: a qualitative study. Chronic Illness 5: 75-91.
- Krenitsky J (2004) Nutrition in renal failure: myths and management. Pract Gastroenterol 28: 40-59.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences