Management and Education in Patients with Diabetes Mellitus
Freddy Contreras, Maria Sanchez, Maria Sofia Martinez, Mervin Chavez Castillo, Andres Mindiola, Valmore Bermudez and Manuel Velasco
DOI10.21767/2471-299X.1000049
Freddy Contreras1, Maria Sanchez2, Maria Sofia Martinez3, Mervin Chavez Castillo3, Andres Mindiola3, Valmore Bermudez3,4 and Manuel Velasco5*
1Internist Medical, MS Science Educational and Management-Educator in Diabetes, Central University of Venezuela, Caracas, Venezuela
2Medical, MS Science Educational and Management-Educator in Diabetes, Medicine School "Luis Razetti" University of Central Venezuela, Caracas, Venezuela
3Endocrine and Metabolic Diseases Research Center, School of Medicine, University of Zulia, Maracaibo, Venezuela
4Advanced Frontier Studies Research Group (ALEF), Simon Bolivar University, Cucuta, Colombia
5“JM Vargas” Medical School, Central University of Venezuela, Caracas, Venezuela
- *Corresponding Author:
- Velasco M
Professor of Pharmacology
“JM Vargas” Medical School
Central University of Venezuela
Caracas, Venezuela
Tel: +58-212-5619871
E-mail: sicontreras2009@gmail.com
Received Date: June 19, 2017; Accepted Date: July 29, 2017; Published Date: August 04, 2017
Citation: Contreras F, Sanchez M, Martinez MS, Castillo MC, Mindiola A, et al. (2017) Management and Education in Patients with Diabetes Mellitus. Med Clin Rev. 3:7. doi: 10.21767/2471-299X.1000049
Abstract
Patients with Diabetes Mellitus (DM) can actively participate in the management of this disease, with therapeutic education playing an essential role in the optimization of knowledge, resources and skills required to achieve targets of metabolic control, reduce the onset of acute and chronic complications, and preserve quality of life. In this context, the management of DM becomes a holistic endeavor, by promoting the reasonable use of therapeutic resources by the patient’s themselves-involving self-management and self-efficacy, their families and their communities, aiming to obtain optimum results. This review summarizes current literature on the active patient-centered management of DM, in order to promote an improvement in these therapeutic goals.
Keywords
Diabetes Mellitus (DM); Management; Therapeutic education; Self-management; Self-efficacy
Introduction
Diabetes Mellitus (DM) is a chronic, progressive, non-communicable disease characterized by an increase in blood glucose secondary to an absolute or relative efficiency in insulin signaling, the major regulating hormone of glycaemia. According to the World Health Organization (WHO) [1] in the 2016 world report on DM, prevalence of this diagnosis and the number of people affected are increasing in the whole world. By 2014, 422 million adults (8.5%) worldwide were estimated to suffer from DM, compared to 108 million (4.7%) in 1980. Indeed, world prevalence (normalized for age) appears to have almost doubled during this period, increasing from 4.7 to 8.5% in adults. In addition, DM accounts for approximately 1.5 million deaths in the world yearly. However, hyperglycemia has been linked to an additional 2.2 million yearly deaths through increased risk for other conditions, in particular Cardiovascular Disease (CVD); 43% of which occur in subjects under the age of 70.
The complications of DM also entail important socioeconomic consequences for the patients and their families, as well as for local and world public health systems, owing to direct and indirect medical costs, which appear to be more severe in developing countries [1]. In Venezuela, Type 2 DM (DM2) represents one of the main causes of morbimortality, with serious repercussions in lifestyle, being closely associated with feeding habits, stress management and sedentary habits, among other determinants [2]. In 2005, the Carmela study [3] found 6% of the Venezuelan population had DM, 5.6% men and 6.3 women. In 2014, Lopez et al. [4] found fasting dysglycemia in 38.95% of a Venezuelan sample, with a prevalence of 14.25% for DM and 40.7% for prediabetes. It was also found that hypertension, hypercholesterolemia, disglycemia and DM were more prevalent in females. In contrast, the WHO report [1] shows an estimated prevalence of 8.8% for DM in Venezuela. The International Diabetes Federation (IDF) estimates, in its 2016 report, a prevalence of 11.1% [5].
Facing this alarming landscape, a plausible option to minimize its impact on the population is disease management through education and prevention, the latter defined by the WHO [6] as “a set of measures aimed not just at preventing the onset of the disease, such as reducing risk factors, but also to stay in advance and attenuate its consequences once established, a goal that may be obtained by giving education to the patient at risk and his/her family group”. This review aims to critically summarize current literature on therapeutic education as a strategy for prevention and treatment in DM.
Management in Diabetic Patients
Paraphrasing Ruiz [7] on the definition of management as the art of handling resources and processes aimed at achieving goals associated with results defined in terms of efficacy and efficiency, it is reasonable to apply the same principle to the management of people with DM. Thus, management of DM implies day-to-day fulfillment of processes leading to optimize resources, skills and abilities, aptitudes and values to attain goals of metabolic control that minimize the onset of acute and chronic complications at the lowest cost and with the best quality of life for patients and family alike.
It is important to underline that management of DM should provide an environment promoting the rational use of human and material resources that play a role in achieving individual health, through a number of practices that promote in patient, family and health providers the achievement of optimum results and intended goals. In general terms, management is considered to be the product of a permanent interaction between thinking and acting, reflection and decision, requiring unique characteristics that define a profile oriented to efficiency, effectiveness and effectiveness in function of the achievement of planned objectives and goals [8].
Because current times demand a medical care model where transdisciplinarity is the norm, it is of utmost importance to establish harmony between laymen, academics, scientists and clinicians, with the firm intention of contributing to the integral formation of patients, family, caregivers and health professionals. This models should actively involve knowledge (cognitive ability), skills (sensory-motor capacity), and aptitudes and values (affective capacity). Accordingly, management of a diabetic must be approached with an integral view that allows optimization of professional resources and encourages a more active role of patients in self-management [9]. This may be reinforced through establishment of norms and protocols that facilitate their widespread application.
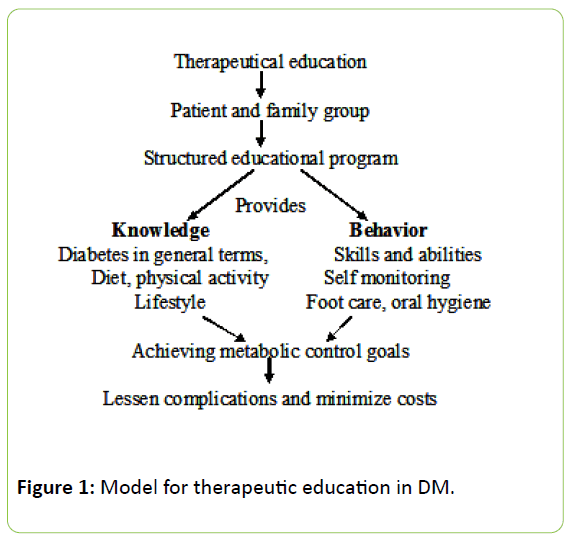
The main goal of this management is to establish an educational program (structured therapeutic education) in a participatory and integral way that, through facilitation or mediation of access to information and knowledge in DM, promotes development of skills and abilities that lead to the promotion of self-responsibility (empowerment) of patients in controlling their clinical condition, in order to achieve optimum metabolic control and thus improve their quality of life. Therefore, it is imperative that educational actions promote permanent self-management, from the time of diagnosis and subsequently as needed.
Thus, the great merit of education in DM would be that through informing and training patients, they will be able to transform their attitudes to the clinical condition. The goal is a shift from a passive approach, consisting of solely following the doctor’s prescriptions, to an active approach, in which the patient becomes a manager or agent responsible and aware of their health situation, with a gradual increase in self-responsibility and personal autonomy in relation to this clinical condition.
Therapeutic Education as a Management Strategy
Therapeutic education involves the set of educational activities essential for the management of chronic diseases, carried out by health professionals trained in the field of education, aiming to assist the patient or groups of patients and their families. The ultimate goal is to enable and empower patients to participate actively in their treatment and prevent avoidable complications, while maintaining or improving the quality of life [10]. Indeed, education is one of the main pillars in the treatment of DM2, as contemplated in the Declaration of Saint Vincent [11], which advocates for the need and importance of continuing education for all those with DM, their families, friends and close acquaintances, as well as the health care team. This proposition arises from the emblematic findings from the DCCT) (Diabetes Control and Complications Trial) study in 1993 [12], which demonstrated that strict metabolic control along with a structured diabetes education program prevented a considerable percentage of chronic complications from diabetes.
Therapeutic education is a dynamic process which evolves and adapts through each of the stages of clinical care, including initial assessment, collection of data obtained at the interview, clinical examination and the findings resulting from biochemical exploration, and establishment of diagnosis or clinical judgment. Therapeutic education should set educational objectives for each of these stages, facilitated by the continuous evaluation of both the process and the results between the healthcare team and the patient and families. This assessment should be systematic and permanent, with the purpose of optimizing the goals of metabolic control and therefore the patient's quality of life [13]. Although there is much evidence to support this idea, only a minority of people receive appropriate therapeutic education [13].
In line with the approaches of the World Health Organization (WHO) (7), health education comprises consciously created learning opportunities, which are a form of communication aimed at improving health literacy, and the population’s knowledge in relation to health, as well as the development of personal skills and self-esteem, activities that will lead to better individual and community health. There is considerable evidence reporting the effectiveness in the short-term (less than 6 months) of educational interventions in the control of DM2 [14-17].
A structured diabetes education program carried out by a multidisciplinary group that works as a team should be able to handle the same terms and maintains the guidelines and goals outlined, achieves that patients improve their metabolic control, adherence to established treatment, changes in diet and physical activity [18]. In addition, recognition of the importance and severity of DM implies considering behavioral factors that may be modified by education of the patient as an indispensable part of the treatment. This should be patient-centered and sensitive to the individual preferences, needs and values of each participant.
The education of both type 1 and type 2 Diabetic Mellitus (DM) should be approadred in the same way concerning therapeutic adherence, nutritional program and participation in exercise physical activities. Hewers in type 1 DM the goods are stricter and it should emphasize concerning adherence and pacification therapeutics to insulin to keep in mind the education to minimize incidence of hypoglycemia.
Empowerment Self-efficiency and Management
Empowerment is a process of transformation by which the individual gains power and control to make decisions and achieve his/her own goals [19]. According to this interpretation, empowerment can be a means to an end (such as reducing poverty or preventing conflict) or can be considered an end in itself (an individual who is empowered). It is important to emphasize that the process happens within the individual and only through his own understanding of reality can change the structures of power.
In this sense, empowerment must be understood as a model, as a strategy of motivation, promotion, awareness and self-management that aims to positively affect the patient. To achieve his/her awareness and appreciation of their condition and how to carry out its management, allowing them to improve their quality of life, through active participation in decision-making and to feel increasingly involved in the process (self-responsibility) and thus achieve the objectives of therapeutics for their own and their family group’s benefit.
Motivations and personal needs, family environment and socio-labor conditions are very important to ensure therapeutic success. The health professional should have the ability to monitor the patient's emotional states, as well as employ adaptive strategies and empathic communication, considering the beliefs, paradigms and perceptions of the patient and their environment. These include discovering in the patient what motivates you to take care of your health, reflect on the things that drive you to continue with diet and exercise. The interrelation with other patients who have achieved success in therapeutics, self-monitoring of their own progress, theoretical and practical knowledge related to diabetes condition, metabolic control goals, success and difficulties of the day to day are factors to have into account in motivating achievement. The motivational force depends on the value that it assigns to the reward and the expectation that it has to achieve it (Self-efficacy).
On the other hand, the social cognitive theory proposed by Bandura [20] defines self-efficacy as the ‘expectation index’ related to being able to perform certain behaviors, which are deemed successful. It is the belief of the person in him and in his ability, which makes him carry out an action. In Bandura’s view, the feelings of self-efficacy directly influence the behavior, so that given the feeling of effectiveness the expected behavior is the result. Self-regulation refers to the ability to control and manage thoughts, emotions or behavior and arises from the beliefs of the subject, which depend on psychosocial development; the person self-regulates by believing in his/her abilities. It is important to emphasize that the processes related to diabetes education are initially affective, later become sensory motor and finally cognitive.
In the same vein, the praxis of self-efficacy requires changing the paradigm of the health professional, from feeling responsible for patients to feel the patients responsible for their clinical condition; that is, responsibility must be transferred to the patient of his own condition. This means that health professionals act as collaborators who provide patients with information, experience and help to make the best possible self-management of DM in each case, with decisions based on the patient's own health priorities and social environment (Figure 1) [21].
Self-management in the Management of Diabetes
Given the complexity of the care a person with DM has to deal with to maintain health and quality of life, it is necessary to promote self-management. It is important that the person incorporates, the term ‘care’ in their daily routine [22]. The common denominator of ‘care’ combines action that requires attention, dedication and effort to conserve life. In this scenario, Orem [23] calls self-care the process that encompasses all activities to promote and maintain well-being throughout life in an independent way. At the same time, he states that carrying out self-care, is based in the capacity that the person has to fulfill those activities.
In agreement with the nature of this care, Kozier et al. [24] affirm that the person implementing self-care has the purpose of preserving their lives and body image, and this means taking responsibility for their health and quality of life, establishing a lifestyle with healthy and self-satisfying alternative behaviors. According to Colliere [22], the nature of care involves healing, and refers to activities related to the need to cure everything that hinders life; requires bringing medicines to cure or eliminate the course of a pathological process (disease). In addition, the person who helps in self-care, being the one who helps and supports (health professional, family, community person) must have clear and precise knowledge of both types of care, their nature and object: the first secures life and the second focuses on the disease, this is important in order not to make exclusions of one from the other [22].
In the context of therapeutic education for the person with diabetes, the family and community participant, Colliere [22], Orem [23] and Luis [25], appeal to the premises of the systems theory, with the purpose of guaranteeing that the person undertakes self-care to satisfy his/her basic and therapeutic needs, determined in the requirements of self-care and its execution. According to this, the existence of three systems is considered: 1) Totally compensatory; 2) Partially compensatory and 3) Educational support. The support-educational system emphasizes that the person with diabetes requires help in decision-making, as well as support in controlling positive and encouraging behaviors to incorporate them in the fulfillment of their self-care. That is, help in acquiring skills to ensure self-monitoring of capillary glycemia, foot care, oral hygiene, insulin administration, adherence to a healthy diet and physical activity.
In relation to the above, Orem [23] and Kozier et al. [24] underline that the person receiving self-care should acquire knowledge about the disease, its natural history, pharmacological treatment and risks and benefits of each action on him/herself. On the other hand, for the understanding and fulfillment of their contributions, it is imperative that caregivers know the culture, religion, beliefs and social landscape of their patients, as well as what the disease represents for them and how it affects the relationships with their environment.
It is important to emphasize that the National Institute of Nursing Research, which is part of the National Institute of Health of the United States, in the eighties proposed the term self-management instead of self-care. In a general sense, self-management is defined as the daily care by the patients themselves of chronic diseases in their course [26,27]. Although it is a term often used as a synonym for self-care, self-management has evolved from being simply the practice of providing information and increasing the patient’s knowledge [28]. Although these concepts are interrelated, self-management is considered by many authors [26,29,30] as the tasks that healthy people perform at home to prevent diseases, rather than just attending to an existing disease.
Conceptual and theoretical descriptions of self-management in relation to components, processes, and outcomes have expanded and evolved since the 1980s when Corbin and Strauss [31] identified three sets of activities associated with having a chronic disease, namely: Medical care, behavior management and emotional management. Nursing scientists subsequently described five major self-management processes that consist of the ability to solve problems, make decisions, use resources, partner with health care providers, and act [27].
Within the theoretical framework of individual and family self-management, it was proposed that self-management has three dimensions: context, process and results, with contextual factors that influence the process and results of selfmanagement practices. This theory also extended the specificity of processes to include knowledge and beliefs, self-regulation skills and capabilities, and social facilitation, and further classified the results into proximal and distal categories [29].
For his part, Pinto [32] proposes a model of home care that he considers fundamental, because it integrates the transpersonal relationship person-caregiver (health professional, family member or community member), exemplifies the process of human-to-human care, and demonstrates the need for a mix of scientific knowledge of the caregiver and the art of intrapersonal experience. It moves toward healthy outcomes, defined as protection and commitment to the well-being of the person and his family at the same time. This continuity demands optimum personal management; Procurement of required and coordinated services; Use of easily accessible technology; Techniques for organizing care or self-care; Development of goals; Compliance and evaluation.
In summary, it requires planning, intervention, monitoring and evaluation of care, to facilitate and monitor the appropriate use of resources over time, encourage feedback and rational communication, accessibility and flexibility of the person and the team. All these are integrated characteristics in each one of the processes developed by the model proposed by Pinto [32]. The American Association of Diabetes Educators, together with Covey [33], proposed the "7 self-care behaviors" (Table 1), which should perfectly develop the patient to achieve greater control of diabetes and all its implications.
| Sl No | Self-care behaviors in patients with DM |
|---|---|
| 1 | Establishment of food patterns appropriate to the individual needs |
| 2 | Be active and practice regular physical activity |
| 3 | Daily monitoring of blood glucose and food care |
| 4 | Pharmacological adherence according to the doctor's instructions |
| 5 | Solve acute problems (hypoglycemia, hyperglycemia) |
| 6 | Psychosocial adaptation and motivation to achievement |
| 7 | Reduce risk of chronic complications |
Table 1: Self-care behaviors [33].
Actions to promote healthy behaviors can be achieved through the following objectives [34]: 1) To improve the patient's lifestyle and behavior towards the disease, to optimize metabolic control (glycemic control and lipids); 2) To guarantee the adhesion to the therapeutics and therefore to prevent the acute and chronic complications; 3) Improve quality of life; and 4) Reduce costs in acceptable ranges.
Nutritional patterns appropriate to individual needs
The ADA and the Diabetes UK establish a degree of recommendation type A that the individuals with prediabetes or diabetes should receive individualized "nutritional medical treatment", necessary to achieve treatment goals, from the time of diagnosis [35]. All members of the health care team should know the principles of nutrition therapy in diabetes and support their unrestrictedly implementation [36].
In this sense, education in Carbohydrate Counting (CHO) is important to patients with DMT1, especially if it involves patients with continuous insulin infusers. People with a mixed insulin regimen, a consistent intake should been considered and a meal simple plan is needed in individuals with oral hypoglycemic or in older adults.
In terms of energy balance, weight control should be the main nutritional strategy for the glycemic control in people with DM who are overweight or obese (type-A evidence). In this sense, the main requirement of a diet plan to lose weight is that the total energy intake should be less than the amount of energy that you drop. In addition, to achieve optimal glycemic control, attention should been focused on total energy consumption rather than on the dietary energy source (macronutrient composition).
Evidence suggests that there is no ideal percentage of carbohydrates, proteins and fats for all people with diabetes; therefore, the distribution of macronutrients should been based on the individualized assessment of dietary patterns, preferences and metabolic goals. The pattern of Mediterranean consumption reported the largest decline in A1C at 1 year (-1.2%) [36].
The ED multidisciplinary team should consider low carbohydrate diets (<130 g/day) not recommended and the dietary CHO should come mainly from foods such: Vegetables, fruits, whole grains, grains and low-fat dairy products (evidence B). In addition, it is important to know the Quality, intrinsic and extrinsic variables, medication/feeding adjustment, CHO count and exchanges (evidence B).
On the other hand, substituting foods with high index or glycemic load for foods of lower index or load can modestly improve glycemic control (evidence C). In general, CHO consumption had recommended between 55-60% of the TCR (total consumption requirement).
On the other hand, it is important to emphasize that protein intake increases plasma insulin values, without significantly altering the glycemic (evidence B) 1 g/kg/day. The total amount should be similar to the general population (15-20% of the TCR). "Hyper-protein" diets have not recommended as a method for long-term to weight loss in people with DM.
In relation to the fats seems to be more important the quality of the fat than the amount (evidence B). Polyunsaturated fats ensure an intake of omega-3s, with the additional benefits reported in decreasing cardiovascular risk and healthy habits (B).
Blue fish consumption should been promoted at least 2 times per week (B). Fatty acids (FA) saturated in proportions less than 7% of the TCR (evidence C), it is recommended to reduce the intake of FA Trans to a range below to 1%. Use phytosterols (1.6-3 g/day).
Additionally, people with diabetes should consume at least the amount of fiber and whole grains recommended for the public (14 g/1000 cal.; 25-40 g per day). (C) High intake of soluble fiber and starches (EASD) brings benefits in blood glucose and lipemia. The recommendation for the general population to reduce sodium to less than 2,300 mg/day is also appropriate for people with diabetes (B).
Nutrition education should guide the consumption of adequate amounts of micronutrients through natural sources. It is very important to familiarize patients, family, caregivers and health professionals with nutritional labeling, portion control, and the exchange list.
Physical activity and diabetes
For the treatment of DM and for the prevention and treatment of cardiovascular problems, it is more convenient to prescribe aerobic than anaerobic exercise, particularly resistance, strength and elasticity exercises, to maintain and improve cardiorespiratory, muscular, Mobility and, indirectly, the body composition [37]. In order that physical activity is safe and beneficial from the outset, a series of previous recommendations should been followed:
1. Detailed medical evaluation is need before beginning any exercise program.
2. Both the patient and the people in his/her environment must know the signs and symptoms of hypoglycemia, and must know how to react to it.
3. Patients should always carry a sugary product and a mobile phone with personal data and emergency numbers.
4. Patients should give special attention to the foot care.
It is recommended that weekly caloric expenditure attributable to physical exercise be at least 1000 calories; it is essential to incorporate into the specific exercise an adequate warm-up and cooling protocol for 5-10 min for the prevention of cardiac arrhythmias, metabolic adequacy, and for the body to adapt to exercise [37].
Beginners should start their exercise plan with activities of 10 to 15 min duration, and progressively increasing the duration of these sessions to 30-60 min/day. As valid as performing that time of exercise in a continuous way is to divide it into several shorter sessions. The type of exercise will depend on the interests and goals of each person, being the truly important motivation is strong enough to maintain adherence to the habit of physical activity and for this, they need a custom clear and compelling recommendations, encouragement and monitoring on the part of the health professionals and particularly of the educators in diabetes.
The low fitness of many patients with DM and coexisting complications introduce changes in the type, intensity, and duration of general recommended activities. Unfortunately, physical activity is, in general, a form of treatment underutilized by diabetics, due mainly to the lack of knowledge of its positive effects and/or lack of motivation. A better education of patients, adequate to each population group, is necessary so that they can overcome the barriers that inhibit their adherence to physical activity as part of a healthy lifestyle. In turn, each person must recognize and be convinced of the benefits that provides perform physical activities on a regular basis. With knowledge and motivation, many diabetics have incorporated physical exercise as an essential part of their lifestyle.
Conclusions
It is necessary to incorporate management, in the quality of care and in the control of diabetes so that patients, the family, the community and health professionals actively participate in an integrated and integrated way, which can become a factor of effectiveness and efficiency.
It should been understood that the transmission of information on the pathophysiological aspects of diabetes and its complications is not the only and exclusive thing to be treated in an educational program. It is imperative to promote education and health promotion by promoting self-efficacy in the context of a clinical condition that can been improved by empowering the individual to achieve effective self-management.
The person with diabetes faces a tough challenge: taking special care of his or her own health and life. Therefore, the inescapable commitment to themselves demands and requires personal care, to provide the body with the necessary requirements to meet a diet, adherence to therapeutic medical and metabolic controls and exercise physical activities, together with the support of the family, the caregivers and educators in diabetes.
Acknowledgements
The authors and researchers wish to express a sincere thanks to the Morella Mendoza Grossman FMMG Foundation for the kind disposition to defray the publication costs of this article. Without this represent a conflict of interest with the content of the same.
References
- World Health Organization (2016) Informe Mundial sobre la Diabetes. WHO/NMH/NVI/16.3.
- Camejo M, Garcia A, Rodriguez E, Carrizales ME, Chique J (2012) Epidemiological overview of diabetes mellitus: situation in Venezuela: epidemiological record and registry proposal. Rev VenezEndocrinolMetab 10: 2-6.
- Schargrodsky H, Hernandez R, Marcet B (2008) Carmela: assessment of cardiovascular risk in seven Latin American cities. Am J Med 121: 58-65.
- Lopez R, Hurtado D, Lopez L, Acosta J, Gerardo Chazzin G, et al. (2014) An approximation to know the prevalence of arterial hypertension, cardiovascular risk factors and lifestyle in Venezuela. AvancesCardiol 34: 128-134.
- FederacionInternacional de Diabetes (2015) Atlas de la diabetes de la FID (7th edn.) (Internet).
- World Health Organization (1998) Promocion de la salud: GlosarioGinebra WHO. Seccion II: Lista de terminos p:15.
- Ruiz J (2000) La gerencia de aula P 12. Venezuela: INSTIVOC.
- Funnell MM, Brown TL, Childs BP, Hass LB, Hosey GM, et al. (2010) National standards for diabetes self-management education. Diabetes Care 33: 89-96.
- Contreras F, Hernandez C, Rivas PIH, Diaz L (2015) Design and implementation of a Diploma in Therapeutic Education in Diabetes (ETD) aimed at health professionals in Venezuela. Vitae 64: 1-12.
- World health Organization Region Office for Europe (1998) Therapeutic patient programmers for healthcare providers in the field of prevention of chronic diseases. Report of a WHO working group. Copenhagen, Denmark.
- https://www.diapedia.org/management/8105473810/the-st-vincent-declaration-on-the-treatment-of-diabetes
- DCCT Research Group (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin dependent diabetes mellitus. N Engl J Med 329: 977-978.
- Grupo de TrabajoGuiasClinicas y Consensos de la Sociedad Espanola de Diabetes (2012) Professional profile of diabetes educator. Av Diabetol 28: 38-47.
- Steinsbekk A, Rygg L, Lisulo M, Rise MB, Fretheim A (2012) Group based diabetes selfmanagement education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. BMC Health Serv Res 12: 1-19.
- Cooper H, Booth K, Gill G (2008) A trial of empowerment-based education in type 2 diabetes global rather than glycemic benefits. Diabetes Res ClinPract 82: 165-171.
- Tshiananga JK, Kocher S, Weber C, Erny-Albrecht K, Berndt K, et al. (2012) The effect of nurse-led diabetes self-management education on glycosylated hemoglobin and cardiovascular risk factors. A meta-analysis. Diabetes Educ 38: 108-123.
- Tang T, Funnell M, Brown M, Kurlander J (2010) Self-management support in “real-world” settings: an empowerment-based intervention. Patient EducCouns 79: 178-184.
- Toro MI (2014) Does self-care and empowerment make the difference in diabetes? ActaMedicaColombiana 39: 224-227.
- Friedman J (1992) Empowerment: The politics of alternative development. Blackwell, Edit. Wiley-Blackwell.
- Bandura A (1989) Social Cognitive Theory. In: Vasta R (ed.) Annals of child development. Six Theories of Child Development 6: 1-60.
- Anderson RM, Funnell MM (2005) Patient empowerment: Reflections on the challenge of fostering the adoption of a new paradigm. Patient Education and Counseling 57: 153-157.
- Colliere MF (1993) Promover la vida. Editorial Interamericana McGraw-Hill. Madrid.
- Orem D (1997) General theory of Orem's nursing. In: Wesley's Theory and Models of Nursing. Editorial Interamericana McGraw-Hill, Mexico pp: 81-86.
- Kozier B, Erb G, Olivieri R (1993) Enfermeria fundamental. Tomo I. Editorial Interamericana McGraw-Hill. Espanapp: 71-72.
- Luis MT (2005) From theory to practice: the thinking of Virginia Henderson in the 21st century (3rd edn.). Editorial Masson, Espana p: 53.
- Clark NM, Becker MH, Janz NK, Lorig K, Rakowski W, et al. (1991) Self-management of chronic disease by older adults: a review and questions for research. J Aging Health 3: 3-27.
- Lorig KR, Holman H (2003) Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 26: 1-7.
- Grady PA, Gough LL (2014) Self-management: a comprehensive approach to management of chronic conditions. Am J Public Health 104: 25-31.
- Ryan P, Sawin KJ (2009) The individual and family self-management theory: background and perspectives on context, process, and outcomes. Nurs Outlook 57: 217-225.
- Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J (2002) Self-management approaches for people with chronic conditions: a review. Patient EducCouns 48: 177-187.
- Corbin J, Strauss A (1985) Managing chronic illness at home: three lines of work. QualSociol 8: 224-247.
- Pinto N (2000) Towards a model of care in the home. In: Nursing care and practice. Universidad Nacional de Colombia. Colombia p: 57.
- American Association of Diabetes Educators, Covey S, Compliments of Bayer Diabetes Care (2003) The 7 habits of highly effective people.
- Contreras F, Leon J, Suarez E (2016) Gestion de la Diabetes Mellitus. Rev Med Interna (Caracas) 32: 228-235.
- Dyson PA, Kelly T, Deakin T, Duncan A, Frost G, et al. (2011) Diabetes UK evidence-based nutrition guidelines for the prevention and management of diabetes. Diabet Med 28: 1282-1288.
- Evert A, Boucher JL, Cypress M, Dunbar SA, Franz MJ, et al. (2014) Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care 37: 120-143.
- American Diabetes Association (2002) Diabetes mellitus and exercise: position statement. Diabetes Care 25: 64-68.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences