Postoperative Infections in Gynecology and Obstetric
William C Rushenge
DOI10.36648/2471-299X.21.7.129
Aymar C Akilimali* and William C Rushenge
Medical student, Faculty of medicine, Official University of Bukavu, Bukavu, South-Kivu, D.R. Congo
- *Corresponding Author:
- Aymar C Akilimali
Medical student, Faculty of medicine, Official University of Bukavu, Bukavu, South- Kivu, D.R. Congo
E-mail: aymarchirimwami@gmail.com
Received Date: March 15, 2021; Accepted Date: March 29, 2021; Published Date: April 05, 2021
Citation: Akilimali AC, Rushenge WC (2020) Postoperative Infections in Gynecology and Obstetric. Med Clin Rev Vol.7 No.3:129
Abstract
The postoperative infections is the common surgical complication in department of Gynecology and Obstetric. The degree of wound contamination and the classification of surgical site infections at the time of surgery plays an important role. The use of antibiotic prophylaxis has significantly decreased but not completely eliminated this undesirable result. Broad spectrum antibiotics should be started as soon as possible upon diagnosis of postoperative infection; most patients respond to treatment within 24 to 48 hours when appropriate antibiotics are selected. Postoperative infections include the vaginal cuff cellulitus, pelvic cellulitus, adnexal infection, ovarian abscess, pelvic abscess, abdominal incision infection and toxic shock syndrome and they are the head of our study.
Keywords
Infection; Gynecology Obstetric; Postoperative; Surgical Site Infection; Wound Classification
Abbreviations: CDC: Centre of Disease Control; Gynec-Obst: Gynecology and Obstetric; SSI: Surgical Site Infection; SSIs: Surgical Site Infections
Introduction
Postoperative infection remains the most common complication of surgical procedures in Gynecology Obstetric [1,2]. In some countries, around of 2% of surgeries result by surgical site infection (SSIs) [1]. The evolution of surgical site infection (SSI) results in considerable patient morbidity [3]. Surgical site infections are between the most common healthcare-associated infection, longer post-operative hospital stays, complementary surgical procedure, and treatment in intensive care units are associated to SSIs [4]. The SSI surveillance protocol count nine types of surgical procedures: coronary artery bypass graft, open and laparoscopic cholecystectomy, open and laparoscopic colon surgery, caesarean section, hip prosthesis, knee prosthesis and laminectomy [5]. Some surgical procedure in Gynec-Obst are interesting in our work.
Surgical site infection in Gynec-Obst., refers to the infection that succeed after surgery in the part of the human body where the surgery is localize. Some between they can sometimes be superficial infections in the skin and others are serious and can concern tissues under the skin. It is also defined as an infection that succeed within 30 days after the surgery. Because most Gynec-Obst. Surgeries are elective, the gynecologist or obstetrician has time to abbreviate microbial inoculum [6,7].
Thus, the objective of the present work was to study the SSI, wound classification and some specifics infections in Gynec- Obst and to indicate some prevention and treatment of specifics infections in Gynec-Obst. Department.
Surgical Site Infection Classification and Diagnosis
The Centre of Disease Control defines SSI as an infection that occurs within 30 days after surgery [6-8]. SSI is a feared complication of surgery. The National Nosocomial Infections Surveillance system set by the CDC graded SSI third amongst all reported cases in nosocomial infections. The incisional group is subdivided into superficial and deep classes. Organ or space infections develop in spaces or organs other than that opened by the original incision or manipulated during the surgical procedure [9,10].
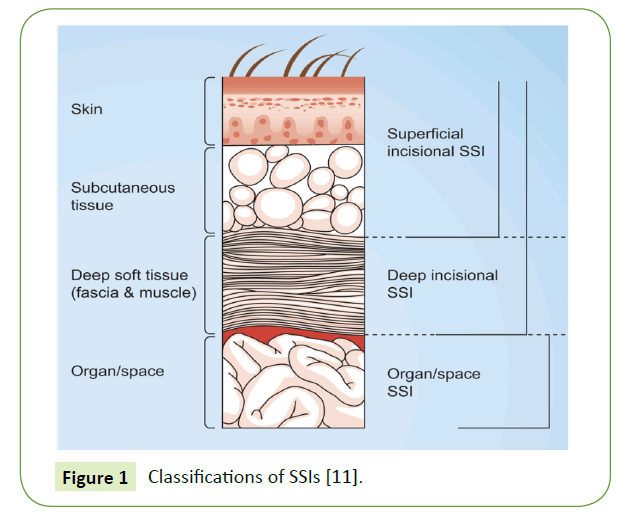
In classification of SSIs, they are two categories, incisional and organ space (Figure 1).
Figure 1 Classifications of SSIs [11].
Criteria for each category and diagnosis are detailed in (Table 1).
| Superficial incisional |
| Concerns only skin and subcutaneous tissue of the incision Develops within 30 days of surgical procedure Features at least one of the following:
Diagnosis of “cellulitis,” by itself, does not meet criterion for SSI. Wound deliberately opened by the surgeon. Surgeon, medical team declare or diagnose as infected. |
| Deep incisional |
| Involves the deep soft tissues (muscle and fascia) of the incision Develops within 30 days of surgical procedure or within 1 year if implant is present Features at least one of the following: purulent drainage from deep incision of surgical site (but not organ or space component), deep incision that spontaneously dehisces or is deliberately opened by a surgeon and is culture-positive (or not cultured) and patient has at least one of the following signs or symptoms: temperature ≥ 38°C and localized pain or tenderness A deep abscess or other evidence of infection found by reoperation, histopathology, or radiology. Surgeon, medical team declare or diagnose as deep incisional infection. |
| Organ/space |
| Involves any body part that was opened or manipulated during the operative procedure, excluding the skin incision, fascia, or muscle layers Develops within 30 days of the surgical procedure or within 1 year if an implant is present Features at least one of the following: Purulent drainage from a drain placed through a stab wound into the organ/space, bacteria obtained aseptically from tissue or fluid in that organ/space and abscess found by reoperation, histopathology, or radiology Vaginal cuff infection with purulence, abscess, and/or positive tissue or fluid culture is included in this category. Surgeon, medical team declare or diagnose as organ and space SSI. |
Table 1 Criteria for defining Surgical Site Infections [12,13].
Wound Classification
Since 1964, surgical wounds have been classified according to the degree of bacterial contamination of the operative site at the time of Gynec-Obst surgery in particular and others surgeries in general. A wound may be defined as any disruption of the integrity of skin, mucous membrane or organ tissue. Wounds can be caused by mechanical, thermal, chemical, and radiogenic trauma [11-14].
Clean wounds are most commonly found in procedures performed or non-traumatic indications, that are without operative site inflammation, and that avoid the respiratory, alimentary and genito-urinary tracts. Thus, most laparoscopic and adnexal surgeries are considered to be in this category. Of these, hysterectomy is the gynecologic procedure most frequently followed by surgical site infection [15].
Contaminated wounds reflect operations with major breaks in sterile technic or incisions in which acute, non-purulent inflammation is encountered. For this reason, a minimum of 24 hours of preoperative antimicrobial administration is required, and delayed wound closure may be selected. Laparoscopy or laparotomy or acute salpingitis is included in this category [6,16- 24]. Dirty wounds are typically old traumatic wounds or those that involve existing clinical infection. If an abscess is present, these are considered dirty wounds [19,20,23,24].
Specific Infections in Gynec-Obst
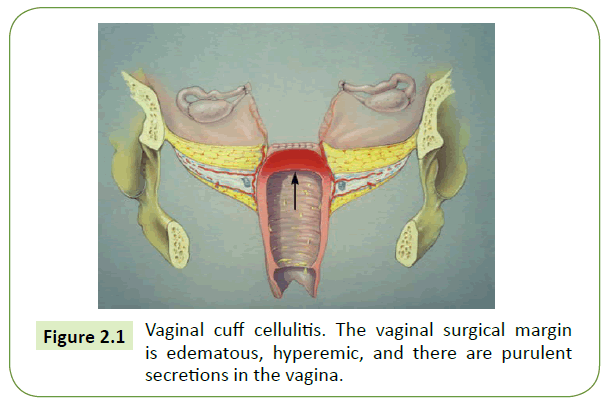
Vaginal cuff cellulitis
Essentially all women develop this infection at the vaginal surgical margin after hysterectomy (Figure 2). Normal response to healing is characterized by small-vessel engorgement, which results in erythema and heat. The few women who do require treatment are usually those who present after hospital discharge with mild, but increasing, new-onset lower abdominal pain and have the yellow vaginal discharge. Findings are as above, but the vaginal cuff is more tender than anticipated at this interval from the initial surgical procedure. Oral antimicrobial therapy with a single Broad Spectrum agent is appropriate (Cephalosporin, Carbapenems, Metronidazole, Clindamycin, etc.) [3,25,26].
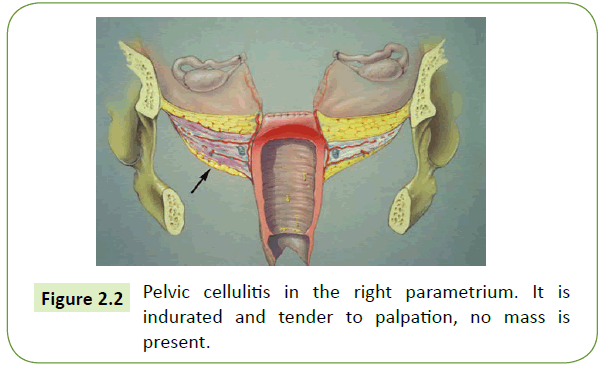
Pelvic cellulitis
An abscess is a defined collection of purulent fluid that has accumulated within the tissues or cavities of organ in the body, this is often a resultants of an infectious process [27].
This is a common infection following either vaginal or abdominal hysterectomy. It develops when host humoral and cellular defence mechanisms, combined with preoperative antibiotic prophylaxis, cannot defeat the bacterial inoculum and inflammatory process at the vaginal surgery [3,28]. Laparotomy with lavage or drainage and surgical incision through the vaginal walls were used as conventional surgical treatment methods for pelvic abscesses [28].
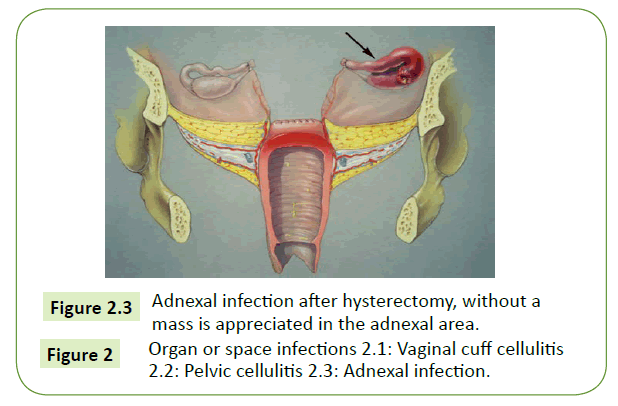
Adnexal infection
This infection is uncommon and present almost exactly like pelvic cellulitis. The difference is in the location o tenderness during bimanual pelvic examination. This infection also may develop after tubal ligation, surgical therapy or ectopic pregnancy, or other adnexal surgery [29].
Ovarian abscess
A rare but life-threatening complication following primarily vaginal hysterectomy is ovarian abscess. Presumably with this infection, surgery is performed in the late proliferative phase of an ovulatory menstrual cycle, and ovaries are in close proximity to the vaginal surgical margin. Affected women have an essentially normal postoperative course until approximately 10 days following surgery. Sepsis commonly follows, and this is a true gynecologic emergency [29].
Infected pelvic abscess or pelvic abscess
Pelvic abscess not involving an adnexal structure may also uncommonly complicate hysterectomy [3].
An alternative infection can originate within a surgical pelvic hematoma. With hematoma, a postoperative-day-1 hemoglobin classically is significantly lower than that predicted by measured intraoperative blood loss [3,27,28].
Abdominal incision infection
The superficial and easily accessible location of this infection aids its diagnosis. Although abdominal incision infection may develop alone or with pelvic infection following abdominal hysterectomy, it develops uncommonly after gynecologic procedures. Drainage and local care are usually the basis of successful therapy or abdominal incision infection [2,3,28,30].
Toxic shock syndrome
This disease are caused by an exotoxin produced by Staphylococcus aureus, appears after 2 days following surgery or menstruation onset. Menstrual-associated toxic shock syndrome rates have diminished following changes in tampon composition and use. For the criteria for diagnosis of Toxic Shock Syndrome, they are the major criteria (hypotension, temperature ≥ 38.8°C, orthostatic syncope, diffuse macular erythrodema, etc.) and the minor criteria (organ system involvement: diarrhea or vomiting, vaginal erythema, bilirubin levels greater than twice normal, etc.) [31].
Prevention of Postoperative Infections in Gynecology and Obstetric
Infection in Gynec-Obst., accounts for the second most common cause of maternal mortality after the postpartum hemorrhage [19]. The cleansing of surgical wounds with sterile saline solution is a common practice among healthcare practicians. As well as improving patient wellbeing, the practice is used to remove excess wound exudate and wound debris. However, the impact this practice might have on SSIs needs more consideration [32].
The purpose of the study was to examine the clinical of using wound cleansing solutions for prevention of SSI in wounds healing by primary and secondary intention.
Surgical site infection prevention recommendations advise these in postoperative period for surgical team and clinical staff actions (do not prolong surgical antibiotic prophylaxis in the postoperative period, do not continue surgical antibiotic prophylaxis due to the presence of a drain and remove wound drain when clinically indicated, evaluate and manage wound appropriately, including cleansing, dressing and care, according to the given wound situation and do not use advanced dressing of any sort or use standard dressings instead) [33,34].
Conclusion
Postoperative infection is a threat to life of the woman and poses a huge problem in Gynecology and Obstetrics. In some countries 2 percent of surgeries in Gynecology and Obstetrics cause infection and the infection is one of the biggest surgical complication. The complication is a function of the conditions under which the surgical intervention takes place as well as the rigor of the aseptic measures in per, intra and postoperative, but also types of procedure during the surgery. Prevention is the best way to fight postoperative infection in Gynecology and Obstetrics by a rigorous asepsis and allows to reduce the mortality rate and the cleansing of surgical wounds with sterile saline solution is a common practice among healthcare practicians.
Conflict of Interest
The authors declare that they have no conflict or interest.
Acknowledgement
We will like to acknowledge the support of Dr. Axel Vedast KATEMBO and PUBRICA for their immeasurable support and professional contribution to the success of this work.
References
- World Health Organisation (2016) : Global guidelines on the prevention of surgical site infection [Internet]. Available from :http://www.who.int/gpsc/ssi-prevention-guidelines/en/
- Pathak A, Mahadik K, Swami MB, Roy PK, Shama M, et al. (2017) Incidence and risk factors for surgical site infections in obstetric and gynecological surgeries from teaching hospital in rural India. Antimicrob Resist Infect Control 14(6): 66.
- Lachiewicz MP, Moulton LJ, Jaiyeoba O (2015) Pelvic surgical site infections in gynecologic surgery. Infect Dis Obstet Gynecol 2015:614950
- European Centre for Disease Prevention and Control. (2019) Healthcare associated infections : surgical site infections. In ECDC. Annual epidemiological report for 2017. Stockholm: ECDC.
- European Centre of Disease Prevention and Control. (2017) Surveillance of surgical site infections and prevention indicators in European hospitals – HAISSI protocol. Version 2.2, Stockholm: ECDC.
- World Health Organization (2018) Protocol for surgical site infection surveillance with a focus on settings with limited resources. WHO Document Production Services, Geneva, Switzerland. ISBN 978-92-4-156554-7.
- European Centre for Disease Prevention and Control (2020) Protocol of Surgical site infection. [Internet]. Available from : http://ecdc.europa.eu/en/publications/Publications/120216_TED_SSI_protocol.pdf
- Campos FSM, Archangelo SCV, Francisco AMC, de Lima RPF, Juliano Y, et al. (2014) Antibiotic Prophylaxis in Gynecologic Laparoscopy: Study Protocol for a Randomized Controlled Trial. J Clin trials 5: 201.
- Onyekwelu I, Yakkanti R, Protzer L, Pinkston CM, Tucker C, et al. (2017) Surgical Wound Classification and Surgical Site Infections in the Orthopaedic Patient. J Am Acad Orthop Surg Glob Res Rev 1(3):e022.
- Lee J, Singletary R, Schmader K, Anderson DJ, Bolognesi M, et al. (2006) Surgical site infection in the elderly following orthopeadic surgery. Risk factors and outcomes. J Bone Joint Surg Am 88:1705-1712.
- Najjar PA, Smink DS (2015) Prophylactic antibiotics and prevention of surgical site infections. Surg Clin North Am 95(2):269-283.
- Centers or Disease Control and Prevention: Procedure-associated module: Surgical site infection (SSI) event. 2014 [Internet]. Available from : http://www.cdc.gov/nhsn/PDFs/pscManual/9pscSSIcurrent.pdf
- Leaper D, Fry D, (2012) Management of surgical site infections. In: Granick M, Teot L, Surgical Wound Healing Management (2nd edition). Informa Healing.
- Kujath P, Michelsen A (2008) Wounds - from physiology to wound dressing. DtschArztebl Int. 105(13):239-248.
- American College of Obstetricians and Gynecologists (2009) Antibiotic prophylaxis or gynecologic procedures. Practice Bulletin No104.
- Nel DC (2014) Surgical Site Infections. S Afr Fam Pract 56(5):33-37.
- Thombare D, Joshi D (2019) A Study of Incidence and Risk Factors in Post Operative Abdominal Wound Infection in Tertiary Care Centre. MVP J Medical Sci 6(1):8-14.
- Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR (1999) Guideline for Prevention of Surgical Site Infection. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control 27(2):97-132
- Amenu D, Belachew T, Araya F (2011) Surgical site infection rate and risk factors among obstetric cases of jimma university specialized hospital, southwest Ethiopia. Ethiop J Health Sci 21(2):91-100.
- CDC/NHSN Surveillance (2017) Definitions for specific types of infections. Atlanta (GA): Centers for Disease Control and Prevention [Internet] Available from : https://www.cdc.gov/nhsn/pdfs/pscmanual/17pscnosinfdef_current.pdf
- Monahan M, Jowett S, Pinkney T, Brocklehurst P, Morton DG, et al. (2020) Surgical site infection and costs in low- and middle-income countries: A systematic review of the economic burden. PLoS ONE 15(6): e0232960.
- Azoury S, Farrow N, Hu Q, Soares K, Hicks C et al. (2015) Postoperative abdominal wound infection – epidemiology, risk factors, identification, and management. Chronic Wound Care Management and Research 2:137-148
- Segal CG, Waller DK, Tilley B, Piller L, Bilimoria K (2014) An evaluation of differences in risk factors for individual types of surgical site infections after colon surgery. Surgery 156(5):1253-60.
- Herman TF, Bordoni B. Wound Classification(2020) In: StatPearls [internet] Treasure Island (FL) : Stat Pearls Publishing.
- Rafal W, Zbigniew F (2006) Contemporary views on perioperative complications and adhaesion formation after vaginal hysterectomy, in relation to peritoneal closure vs. Non closure in combination with open vs. Closed vaginal cuff. Ginekol Pol 77(12):973-979
- Adejumo A, Nuhu M, Afolaranmi T (2015) Incidence and risk factors of abdominal surgical site infection in Nigerian Tertiary Health care centre. IJIC 11(4).
- Elkbuli A, Kinslow K, Diaz B, Hai S, McKenney M, Boneva D (2019) Giant pelvic abscess with sepsis: Case report and review of current literature. Int J Surg Case Rep 64:85-88.
- Akinci D, Ergun O, Topel Ç, Ciftci T, Akhan O (2018) Pelvic abscess drainage: outcome with factors affecting the clinical success. Diagn Interv Radiol 24(3):146-152.
- Sayan CD, Yeral MI, Ozkan ZS, Karaca G, Asal N et al. (2018) Sigmoid Colon Perforation Mimics a Tuboovarian Absces. Med Arch 72(2):151-153
- Khaliq K, Nama N, Lopez RA. Pelvic Abscess (2020) In: Stat Pearls [Internet]. Treasure Island (FL): Stat Pearls Publishing.
- Ross A, Shoff HW. Toxic Shock Syndrome(2020) In: Stat Pearls [Internet]. Treasure Island (FL): Stat Pearls Publishing.
- National Collaborating Centre for Women’s and Children’s Health. August 2020. Prevention and treatment of Surgical site infection. ISBN 978-1-904752-69-1
- World Health Organization (2018) Preventing surgical site infections: implementation approaches for evidence-based recommendations. ISBN 978-92-4-151438-5
- Pellegrini JE, Toledo P, Soper DE, Bradford WC, Cruz DA et al. (2017) Consensus Bundle on Prevention of Surgical Site Infections After Major Gynecologic Surgery. AANA J 85(1):1-12.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences