COVID-19 vs. Children: A Discussion of the Potential Factors Causing the Decreased Mortality in the Infected Children
Sandra Abboud and Sarah Kassem
Sandra Abboud* and Sarah Kassem
Department of Radiology, Faculty of medicine, Damascus University, Lebanon
*Corresponding Author:
Sandra Abboud
Department of Radiology
Faculty of medicine, Damascus University, Lebanon
E-mail: sandraabboud000@gmail.com
Received Date: August 15, 2020; Accepted Date: September 15, 2020; Published Date: September 22, 2020
Citation: Abboud S, Kassem S (2020) COVID-19 vs. Children: A Discussion of the Potential Factors Causing the Decreased Mortality in the Infected Children. Med Clin Rev. Vol. 6 No. 4: 101.
DOI: 10.36648/2471-299X.6.4.101
Abstract
Abstract
Background: In this paper we will discuss the recent global pandemic, the COVID19 comparing between its effect on both adults and children and review the relation between its occurrence and two previous pandemics caused by a corona family virus in 2003 and 2013.
Method: we can divide the topic into two parts, the first part we talked about reasons that make children less symptomatic. First, the virus requires a special type of receptors on the surface of cells in the body known as ACE-2 cells, another aspect is the viral load, and finally, the cytokine storm.
In the second part we discussed the relation between this new virus and the two previous pandemics the SARS (sever acute respiratory syndrome) in 2003 and the MERS (middle east respiratory syndrome) in 2013 to reach to our point of the new reason that make children less affected from this new virus.
Noting that we are analyzing the link between the previous pandemics and the current one regarding the number of reported cases in each country, and not the number of deaths or recovered cases.
Result: Because of these two past exposures of coronavirus, adults who were exposed to this past coronavirus created memory antibodies against it. The new idea suggests that these antibodies which were formed, in many times they are not exactly matched to the new coronavirus and that can affect negatively, so these antibodies instead of helping the body defend against this new virus, they damage it.
Conclusion: That suggests the idea that children who were not born during that time, and therefor were not exposed to the viruses nor formed antibodies against it and therefore cytokine storm, developed considerably less severe symptoms or, in some cases, no symptoms.
Keywords
COVID19; Children; SARS; MERS; Pandemic; Coronavirus
Introduction
The SARS-COV-2 virus, also known as COVID-19, is a Corona family member that has emerged in 2019 in China. It is a respiratory virus that can be transmitted through droplets from an infected person to a healthy one. It has become the defining feature of 2020, so far. Until June 2020, there have been 5.8M cases and 360K deaths. According to WHO, a typical human coronavirus has an incubation period of 3-14 days [1]. During this period, symptoms in adults can vary between mild cough and lethargy to ARDS (Acute Respiratory Distress Syndrome). And in other cases, the disease may lead to death. On the other hand, it has been noted that the disease less affects children than adults [2,3], even when infected. Still, the reported cases were accruing in older children and adolescents [4] and when it occurs, it is mostly comorbidity [5,6]. Also, the reported cases of infected children seemed to be mostly asymptomatic or presenting with mild symptoms. Even if moderately severe, it tends to resolve within a couple of weeks [7]. The percentage of affected children who had mild to no symptoms was 90% [8].
Method
And the question is "why don't children seem to get very ill from the coronavirus?"
Main reasons
We have obtained several trusted sources of information. We shall receive and understand the presented data thoroughly, discuss the available information, and reach a logical conclusion.
For now, we will discuss three aspects:
First, the virus requires a special type of receptors on the surface of cells in the body known as ACE-2 cells; it is a specific protein that allows the virus to infect human cells like a key being inserted into a lock. In general, ACE2 is present in many cell types including the lungs, heart, blood vessels, kidneys, liver and gastrointestinal tract [9]. Comparing with children, several studies suggest the presence of fewer receptors in children's lungs, and more in the upper respiratory tract, causing them to present less severely. Some studies suggest that age-related to expression and has portability to link to Covid19virus [10,11]. Another aspect is the viral load. It has been mentioned that asymptomatic patients had many factors contributing to their lack of symptoms; one of them is the viral shedding. Asymptomatic patients have a shorter duration of viral shedding as noted in their nasopharynx swabs when obtained [12]. Last but not least, the cytokine storm. It is an immune response activated in ill adults to fight off any virus enter to the body and eliminate it. In our virus we notice that this method, instead of helping the body to stay strong it causes multiple organ failure like ARDS then death [13].
Background research
However, in children it does not seem to cause as much trouble, which suggests that there is something fundamentally different, exist in adults neither than in children. According to the history of coronavirus, we noticed that in the past we had two pandemics in two different years, which are Severe Acute Respiratory Syndrome (SARS) in 2002 and Middle Eastern Respiratory Syndrome (MERS) in 2012. However, what they had done throughout these years and how they had affected on the new coronavirus?
Statistical analysis
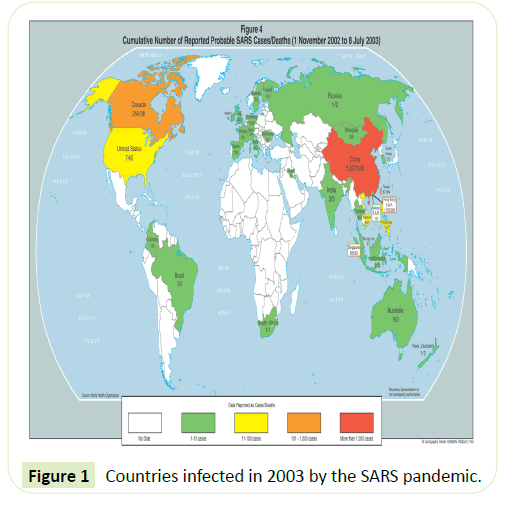
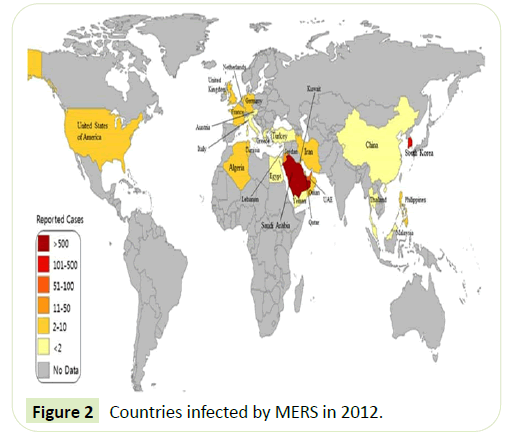
These two tables (Tables 1 & 2) show us the countries infected by the two old pandemics SARS in 2003 and MERS in 2013. We notice that SARS located in China then had spread to Hong Kong, Canada, Taiwan, Singapore, and Europe in general. While MERS first located was in Saudi Arabia then it had taken place in other countries like South Korea, United Arab Emirates, Jordan, Qatar, and also in Europe but in fewer cases unlike SARS. By calculating the correlation coefficient between these pandemics, we conclude a mild relation between MERS and COVID-19, and a stronger, but still mild, relation between SARS and COVID-19. A relation, however small, considered statistically significant.
Table 1 MERS confirmed cases and deaths From June 2012 to January 2020.
| Cases | Deaths | Fatality | |
|---|---|---|---|
| WHO total as of Jan 2020 | 2519 | 866 | 34.30% |
| Reported confirmed cases per country | |||
| Saudi Arabia | 1029 | 452 | 44% |
| South Korea | 184 | 38 | 20% |
| United Arab Emirates | 74 | 10 | 14% |
| Jordan | 19 | 6 | 32% |
| Qatar | 10 | 4 | 40% |
| Oman | 5 | 3 | 60% |
| Iran | 5 | 2 | 40% |
| United Kingdom | 4 | 3 | 75% |
| Germany | 3 | 1 | 33% |
| Kuwait | 3 | 1 | 33% |
| Tunisia | 3 | 1 | 33% |
| Algeria | 2 | 1 | 50% |
| France | 2 | 1 | 50% |
| Spain | 2 | 0 | 0% |
| Netherlands | 2 | 0 | 0% |
| Philippines | 2 | 0 | 0% |
| United States | 2 | 0 | 0% |
| Greece | 1 | 1 | 100% |
| Malaysia | 1 | 1 | 100% |
| Turkey | 1 | 1 | 100% |
| Yemen | 1 | 1 | 100% |
| Austria | 1 | 0 | 0% |
| Egypt | 1 | 0 | 0% |
| Italy | 1 | 0 | 0% |
| Lebanon | 1 | 0 | 0% |
| Thailand | 1 | 0 | 0% |
| Reported total | 1360 | 527 | 39% |
Table 2 Probable cases of SARS by country or region, 1 November 2002-31 July 2003.
| Country or region | Cases | Deaths | Fatality (%) |
|---|---|---|---|
| Australia | 6 | 0 | 0 |
| Brazil | 3 | 0 | 0 |
| Canada | 251 | 43 | 17.1 |
| China | 5,327 | 349 | 6.6 |
| Colombia | 1 | 0 | 0 |
| France | 7 | 1 | 14.3 |
| Germany | 9 | 0 | 0 |
| Hong Kong | 1,755 | 299 | 17 |
| India | 3 | 0 | 0 |
| Indonesia | 2 | 0 | 0 |
| Ireland | 1 | 0 | 0 |
| Italy | 4 | 0 | 0 |
| Kuwait | 1 | 0 | 0 |
| Macau | 1 | 0 | 0 |
| Malaysia | 5 | 2 | 40 |
| Mongolia | 9 | 0 | 0 |
| New Zealand | 1 | 0 | 0 |
| Philippines | 14 | 2 | 14.3 |
| Romania | 1 | 0 | 0 |
| Russia | 1 | 0 | 0 |
| Singapore | 238 | 33 | 13.9 |
| South Africa | 1 | 1 | 100 |
| South Korea | 3 | 0 | 0 |
| Spain | 1 | 0 | 0 |
| Sweden | 5 | 0 | 0 |
| Switzerland | 1 | 0 | 0 |
| Taiwan | 346 | 73 | 21.1 |
| Thailand | 9 | 2 | 22.2 |
| Total (29 territories) | 8,096 | 774 | 9.6 |
| Total excluding China[a] | 2,769 | 454 | 16.4 |
| United Kingdom | 4 | 0 | 0 |
| United States | 27 | 0 | 0 |
| Vietnam | 63 | 5 | 7.9 |
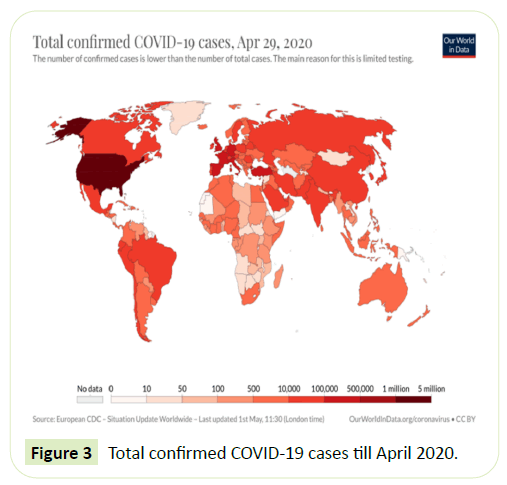
If we across this finding we find that there is no relation between these pandemics but, if we take the COVID19 (Table 3) in our mind we will reach to our suggestion which is, the different spread of these two pandemics helped this new corona virus in his dominate all over the world in this high speed.
Table 3 Characteristof zoonotic coronavirus strains MERS-CoV, SARS-CoV, SARS-CoV-2, and related diseases.
| MERS-CoV | SARS-CoV | SARS-CoV-2 | |
|---|---|---|---|
| Disease | MERS | SARS | COVID-19 |
| Outbreaks | 2012, 2015, 2018 | 2002-2004 | 2019-2020 pandemic |
| Epidemiology | |||
| Date of first identified case | Jun 2012 | November 2002 | December 2019 |
| Location of first identified case | Jeddah, Saudi Arabia | Shunde, China | Wuhan, China |
| Age average | 56 | 44 | 56 |
| Sex ratio (M:F) | 3.3:1 | 0.8:1 | 1.6:1 |
| Confirmed cases | 2494 | 8096 | 7,547,702 |
| Deaths | 858 | 774 | 422;062 |
| Case fatality rate | 37% | 9.2% | 5.591927% |
Result
By cross-referencing the data at hand, we can note that. Because of these two past exposures of coronavirus, adults who were exposed to this past coronavirus created memory antibodies against it. As we know, every virus enters the body causes the creation of antibodies that help in defending the body in the second entry. By reviewing the maps that were presented, we noticed that adults who lived during the pandemics of 2003 and 2013, were exposed to the viruses and formed the mentioned antibodies [14].
The new idea suggests that these antibodies which were formed, in many times they are not exactly matched to the new coronavirus and that can affect negatively, so these antibodies instead of helping the body defend against this new virus, they damage it “sometimes unmatched antibodies can be more harmful than good”, says Wendy Barclay at Imperial College London. That suggests the idea that children who were not born during that time, and therefore were not exposed to the viruses nor formed antibodies against it, developed considerably less severe symptoms or, in some cases, no symptoms. for some reason, younger children don’t seem to mount the aggressive immune response (known as a “cytokine storm”) in response to the virus that adults do; it’s this intense immune reaction that can act as friendly fire in the lungs and make breathing difficult. Why children don’t have hyper-reactive immune responses isn’t clear yet, but it might be because their systems aren’t primed to launch such a powerful response [15]. Also, considering the increased number of people who travel globally which means more and more exposure [16].
Discussion
If we examine the countries infected in 2003 by the SARS pandemic (Figure 1) [17] We notice that most cases have been dominated in China, Canada, United States and Europe. And the countries infected by MERS in 2012 (Figure 2) [18].
According to WHO:
Approximately 80% of human cases reported by the Kingdom of Saudi Arabia. Cases identified outside the Middle East are people who were infected in the Middle East and travelled to other countries (Figure 3) [19,20].
Conclusion
That suggests the idea that children who were not born during that time, and therefor were not exposed to the viruses nor formed antibodies against it and therefore cytokine storm, developed considerably less severe symptoms or, in some cases, no symptoms.
Funding
The authors declare that they have no funding.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
The authors declare that they have no informed consent.
References
- https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html
- Dong Y, Mo X, Hu Y, Qi X, Jiang F, et al. (2020) Epidemiology of COVID-19 Among Children in China. Pediatrics 145: e20200702.
- de Lusignan S, Dorward J, Correa A, Jones N, Akinyemi O, et al. (2020) Risk factors for SARS-CoV-2 among patients in the Oxford Royal College of General Practitioners Research and Surveillance Centre primary care network: a cross-sectional study. Lancet Infect Dis 20: 1034-1042.
- Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P (2020) Hyperinflammatory shock in children during COVID-19 pandemic. Lancet 395: 1607.
- CDC COVID-19 Response Team (2020) Coronavirus Disease 2019 in Children - United States, February 12-April 2, 2020. MMWR Morb Mortal Wkly Rep 69: 422.
- Patel PA, Chandrakasan S, Mickells GE, Yildirim I, Kao CM, et al. (2020) Severe Pediatric COVID-19 Presenting With Respiratory Failure and Severe Thrombocytopenia. Pediatrics 146: e20201437.
- https://www.uptodate.com/contents/coronavirus-disease-2019-covid-19-considerations-in-children
- Dong Y, Mo X, Hu Y, Qi X, Jiang F, et al. (2020) Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics.
- Weston S, Frieman MB (2020) COVID-19: Knowns, Unknowns, and Questions. mSphere.
- https://pediatrics.aappublications.org/content/pediatrics/
- Lee PI, Hu YL, Chen PY, Huang YC, Hsueh PR (2020) Are children less susceptible to COVID-19? J Microbiol Immunol Infect 53: 371-372.
- Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy 75: 1730-1741.
- https://www.who.int/emergencies/mers-cov/en/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7194613/
- https://www.infezmed.it/index.php/article?Anno=2020&numero=2&ArticoloDaVisualizzare=Vol_28_2_2020_174&fbclid=IwAR2_zCFJnOz0nx8rJqMmVricPcFlSJX0fB5vA0vSIMZmagDosj3VMZTbc3k
- https://www.statista.com/statistics/186743/international-tourist-arrivals-worldwide-by-region-since-2005/
- https://www.bbc.com/future/article/20200330-coronavirus-are-children-immune-to-covid-19
- https://ourworldindata.org/app/uploads/2020/05/total-cases-covid-19-12-768x542.png
- https://www.researchgate.net/profile/Masaud_Shah/publication/281293335/figure/fig1/AS:281319876644905@1444083293543/Global-distribution-map-of-Middle-East-respiratory-syndrome-coronavirus-MERS-CoV.png
- https://ourworldindata.org/app/uploads/2020/05/total-cases-covid-19-12-768x542.png

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences