Cytomegalovirus colitis and Comparing the Treatment of Ulcerative Colitis, CMV Colitis, and Co-Colitis
Bingqiang Zhang* and Satish Chandra yadav
DOI10.36648/2471-299X.7.2.119
Bingqiang Zhang* and Satish Chandra yadav
Department of radiology, Faculty of medicine, Damascus University, Lebanon
- *Corresponding Author:
- Bingqiang Zhang
Department of Gastroenterology, Chongqing medical university, Chongqing, China
E-mail: zhbingqiang@163.com
Received Date: January 27, 2021; Accepted Date: February 24, 2021; Published Date: March 03, 2021
Citation: Zhang B, Yadav SC (2020) Cytomegaloviruscolitis and Comparing the Treatment of Ulcerative Colitis, CMV Colitis, and Co-Colitis. Med Clin Rev Vol.7 No.2:119
Abstract
Cytomegalovirus can attack different body parts like colon, salivary gland, eye, lungs, kidneys, etc. The connection between ulcerative colitis and Cytomegalovirus has been established for more than half century but still remains a hot topic of discussion. It is still not obvious whether CMV is a contributor or a bystander. Cytomegalovirus can attack colon causing CMV colitis whose symptoms are similar to ulcerative colitis or both colitis may occur together at same time, so it is really difficult and important to recognize and treat as early as possible to prevent the surgery or mortality. UC can be treated with immunosuppressive drugs while CMV colitis is treated with anti-viral drugs but Co-colitis if treated with immunosuppressive drugs can further deteriorate immunity letting virus to worsen its effect and diseases.
Keywords
Cytomegalovirus; Ulcerative colitis; CMV colitis; Co-colitis
Introduction
CytomegalovirusColitis (in short CMV colitis) is an inflammatory bowel disease caused by Cytomegalovirus (CMV). Cytomegalovirus (CMV) is a double-stranded DNA virus, along with human herpes virus, Epstein -Barr virus, Varicella- Zoster virus, Herpes Simplex virus belongs to Herpesviridae family [1]. Its prevalence rate is more than 70%in human beings [2]. The spectrum of disease varies according to the immunity of the host. The immune competent patients are asymptomatic and may carry lifelong latent infection, whereas the immunocompromised patients with human immunodeficiency virus [3] and transplant recipients [4], have greater morbidity and mortality rate. The relation between ulcerative colitis and CMV colitis is more than 50 years [5] old; these have a multifaceted relationship linking a diagnostic group of bowel diseases. In the present article, we review the general concept about Cytomegalovirus and CMV colitis along with that we focused mostly in the treatment of ulcerative colitis, CMV colitis, and co-colitis.
History, Epidemiology and Transmission
Cytomegalovirus was first isolated in human salivary gland by 3 different independent groups in 1956 [6-8] and it was called as salivary gland virus. In 1960, Weller, et al coined a term Cytomegalovirus [9]. Powell, et al found the association between CMV and Ulcerative Colitis in 1961 [5]. Since the first report, it has been suggested that there is a correlation between these two diseases; however, Weather one can predispose to the other, or whether CMV is just an “innocent bystander,” remains controversial [10].
The prevalence of CMV infection varies with age, race, ethnicity, and socioeconomic status. Two study found that prevalence was highest in older patients and lowest in younger [11,12]. The prevalence is higher in Asian and African compared to European and American [13]. One study shows that CMV positive was found more in women, large size family, low economic status, illiterate people [14]. The prevalence of Cytomegalovirus is found in new onset UC cases, severe UC, steroid refractory UC, nonrefractory colitis even leading to colectomy. The prevalence of CMV infection in UC cases were found 4.5% in new onset UC by Kim et al [15] and 13.8% in severe UC by Kambham et al [16], 27.3% in steroid refractory UC by Maconi G. et al [17] and 9.1% in non-refractory colitis cases by Kim YS et al [18] in their respective study. A study from Africa found that up to 14% patients with HIV and CMV co- infection had GI tract symptoms due to CMV [19]. The seroprevalence of Cytomegalovirus reactivation is severe colitis case is about (4.5-16.6)%, among them 25% cases needed surgery [20].
CMV can be found in urine, blood, throat, cervix, semen, stool, tears, and breast milk [21,22]. The transmission of CMV infection from person to person varies different routes. The prevalence is higher in a person with multiple sexual partners [23]. It can be transmitted with close contact to infected person as the prevalence is higher in family member [24] and daycare centers [25]. It can also be transmitted with transfusion of blood and blood products [26-28] transplantation of organs [29] from seropositive donors, from mother transplacentally or during birth or during breast feeding [30,31]. CMV can be viable in open area for several hours. Stowell, et al in their study took a sample saliva containing CVM and kept them on different surface and they reevaluated the samples by culture and real-time PCR, their result shows that CMV can be alive on metal and wood for 1 h, 3 h on glass and plastic, and 6 h on clothes, rubber, and cracker [32].
Pathogenetic Mechanisms of CMV
Cytomegalovirus is a DNA virus with double-strand and belongs to herpes family (HHV-5).The Transmission of Cytomegalovirus usually occurs through body fluids such as blood, saliva, milk, urine, tear and vaginal fluids. Cytomegalovirus enters the human cell by phagocyctic process or by fusion with cell membrane. Inside the nuclear membrane of nucleus, Cytomegalovirus particles are made and envelope shapes are formed. Inside the trans- Golgi network pathogenetic properties of virus is obtained by proteolytic cleavage of a furin site by forming glycoproteinB(gB). The CytomegalovirusUL55gene product is GlycoproteinsB, which is predominant in virus envelope. GlycoproteinsB have capacity to cleave many proteins like serum proteins, metalloproteinases, exotoxins, growth factors and glycoproteins [33,34].
Cytomegaloviruses have greatest number of the gene which can alter the immune defense of the host. Cytomegalovirus can escape the host immune defense and detection by number of the mechanisms such as by inhibiting cytokines production, by inhibiting apoptosis of infected cells, by binding with CMV-produced Fc receptors, blocking antigen of Major Histocompatibility Complex (MHC) molecules class I and II, by inhibiting Natural Killer (NK) cells function [35-38]. Inside the macrophage, endothelial cells and granulocyte cells Cytomegalovirus become latent to escape host defense in immunocompetent hosts. In immunocompromised patients the humeral immunity usually produces anti-CMV antibodies. T-cell function is directly related to severity of disease [39,40]. IBD patients have weak immune capacity may be due to decrease function of NK cells or poor nutrition or due to medications. In these kinds of patients, virus are reactived by TNF-a, proinflammatory prostaglandins and catecholaminesm [41-44].
The major pathophysiologic steps in IBD is the local expression of the cytokines such as IL-2, IFN-γ, and TNF-a. Dendritic cells and monocytes cells help in virus replication because of chemokines production; transcription factors (NF-Kb) activation leads these cells into inflamed area. T-cells are stimulated by endothelial cells to produce IL-2 and acts as permissive cells and proliferate. Activated T-cells produce IFN-γ and TNF-a, which causes inflammation and injury to tissue [45,46]. Th1 and Th17 are the major cytokines of CD arise due to differentiation of CD4+ T-cell [47,48]. CMV infection in CD patient is efficiently eliminated due to Th1 (IF-γ) and local response of T-cell against Cytomegalovirus.
Th2 is major cytokines in UC [49], which help Natural Killer T- cells to produce IL-13. Th2 cannot efficiently eliminated or deactivate virus replication due to lack of effective cytokines so most of case in clinic, we see is CMV superimposed on UC not CD.
Symptoms and Sign
Immunocompetent patients have no any symptoms so they are unaware that they have been infected with CMV. Primary symptoms are fever, fatigue absolute lymphocytosis and atypical lymphocytes which is also called mononucleosis symptoms.21In immunosuppressed patient CMV colitis and UC have similar symptoms, that is diarrhea, weight loss, hematochezia, abdominal pain, tenesmus , malaise, anorexia, and fever [50].
Perforation, massive bleeding, CMV infection in organ transplant or co-infection with IBD increase the risk of morbidity and mortality significantly [51,52].
Diagnosis
CMV can be diagnosed by taking clinical history, physical examination, serology, histology, culture, antigen testing, DNA testing and endoscopy. The advantages and disadvantages of each method vary as shown in Table 1.
| Test | Source | %Sensitivity | %Specificty | Remarks |
|---|---|---|---|---|
| Serology | ||||
| IgG | Blood | 98-10055 | 96-9955 | Fast, cheap, past repots may not be available to compare, for intestinal disease less specific |
| IgM | Blood | 10055 | 9955 | Quick, economical, highly sensitive, low specificity for intestinal disease, undetectable in active stage |
| Antigen | Blood, CSF | 60-100 58,59 | 83-100 58,59 | Rapid, systemic, semiquantative, more and experience technician needed, test should be done within 6hours,undetected in neutropenic patient |
| PCR test | ||||
| Blood | 65-10059,63,64 | 40-9259,63,64 | Positive predictive value is 94.5% and Negative Predictive Value is 87.4% correlated with active disease | |
| Tissue biopsy | 10067 | 6667 | Highest accuracy, Positive test indicates active CMV but may not be symptomatic | |
| Shell vial assay | Biopsy | 42.869 | 98.4569 | Fast, semiquantative, Positive predictive value is 87.6% and Negative Predictive Value is 86.9% |
| Histology | ||||
| Hematoxylin and Eosine (H and E) | Biopsy | Oct-55 | 92-10055 | Cytomegalic cell, number of biopsy, inexpensive, insensitive, sampling error |
| Immunohistochemistry(IHC) | Biopsy | 78-9355 | 92-10055 | Cytomegalic cell, number of biopsy, costly ,not sensitive, sampling error |
| Viral culture | Blood, Biopsy | 45-7855 | 89-10055 | Time consuming 1weeks to 3 weeks, high false negativity |
Table 1 Diagnosis of CMV Colitis.
Serology test
Blood serology test is a fast and cheap test which is very helpful in identifying patients, who are at the risk of CMV infection because CMV infection can only be found in those patients who are anti-CMV (IgG antibodies +VE) [53,54]. At least, 4-fold increase in IgG antibody between 2 weeks to 4 weeks apart is the diagnostic criteria of CMV infection but most of the patients with severe colitis did not have past IgG test reports available. IgGtest is very sensitive (98-100)%and specific (96-99)% for CMV infection [55]. IgG does not change in reactivation phase so it cannot distinguish between CMV carrier and CMV reactivation. IgMantibody will increase after 14days to 40 days after infection and decrease after 2months to 3 months of infection and cannot be detected after 12 months of infection so patient with active CMV infection, IgM antibody may not be detected at all. IgM test have sensitivity of 100% and specificity is only 99% as it is not so specific for disease of colon [55,56].
Antigen test
This test is done in blood, CSF, saliva and urine .it is systemic test which is rapid but semiquantative. It detect pp65 viral antigen in neutrophils of white blood cells [57]. This test need intensive labour and trained technician to perform mRNA amplification or immunofluorescence assay. The sensitivity of this test is (60-100)%, but sensitivity decreases as time goes over 6 h and specificity of this test is (83-100)% [58,59]. It does not distinguish between latent or active infection and generally found during replication phase [60]. This test is not specific for intestinal disease and antigen is not detected in leukopenic patient [61,62].
PCR test
This test is used to detect the DNA or RNA of CMV virus. This test can be either qualitative or quantitative. Quantitative test is more sensitive that qualitative test. This test is done in blood, stool and tissue biopsy. This test is very fast and most sensitive, positive reports indicate active disease but may not be symptomatic.
Blood: the sensitivity of PCR test in blood is (65-100)% and specificity is (40-92)% [59,63,64]. In one study, it shows that viral load more than 1000 copies per 100000 leukocytes dose indicate symptomatic infection of CMV [65]. In another study Kandiel, et al. state that viral load more than 25 copies per Milliliter (Ml) of whole blood is level to start antiviral drugs [55].
Faeces: Some new study shows PCR test can be done in human stool in CMV colitis patient. It is noninvasive method so its higher sensitivity and specificity is good news for us but detail study is yet to be done [66].
Colonic mucosa: This test is done in patient with severe UC not responding to conventional treatment. This test has higher accuracy to find the virus. The sensitivity of this test is 100% but specificity is only 66% because of false positive [67]. There should be certain limit to diagnose CMV infection and to start antiviral treatment, Roblin et al. proposed viral load more than 250 per microgram in tissue biopsy sample [68].
Shell vial assay
This test is done with sample containing CMV, placed in shell vial and centrifuged in incubator at a low speed. After 1day to 2 days cell are stained with anti-CMV labeled fluoresce in antibody and observed under fluorescent microscope. This method is fast within 24 h to 48 h, semiquantative, active disease are indicated my positive reports. This test should be performed with 6 h else sensitivity will decrease. Sensitivity and specificity of this test is 42.8% and 98.45% respectively [69] and Positive predictive value and negative predictive value is 87.6% and 86.9% respectively.
Histology
There are two methods Hematoxylin and Eosine (H and E) and Immunohistochemistry(IHC).This is the gold standard method to diagnose CMV colitis.
Hematoxylin and Eosine (H and E)
Colonic biopsy are taken and stained and observed under microscope. The cell is 2 times to 4 times bigger than surrounding cells. These cells have thicker nuclear membrane and large intracyotplasmic granular inclusions. This cell is surrounded by halo giving appearance like owl’s eyes. Sensitivity and specificity of this test is 10% to 87% and 92% to 100% respectively [55]. Sometimes it is very difficult to find this cell, need deep mucosal biopsy and experience pathologist. We should avoid sampling error for better result.
Immunohistochemistry(IHC)
This test have better Sensitivity 78% to 93% than Hematoxylin and Eosine (H and E) and similar specificity 92% to 100% to Hematoxylin and Eosine (H and E) test [55]. Monoclonal antibody is used against viral antigen gives better diagnosis reports.
Viral culture
CMV can be cultured from blood sample, tissue biopsy, urine and saliva. This test was considered as the gold standard test in the past but now it is no longer used in clinical practice because we have now better methods, which gives better result compared to this test. It takes 1weeks to 3 weeks to culture virus so it is time consuming process. The Sensitivity and specificity of this test is 45% to 78% and 89% to 100% respectively [55]. This test should be done with 6 h of sample taken. It has high false negativity result.
Endoscopy
The endoscopy tests help us to see the lesion and to take the biopsy, which lead to better diagnostic result. The gross finding is similar to IBD. The endoscopic finding shows patchy erythema, exudates, diffusely edematous mucosa, microerosions, deep ulcers, false tumor or similar to false membrane colitis. Generally right side of the colon is affected [70]. CMV can also be found in mucosa that looks normal grossly [71].
Treatment
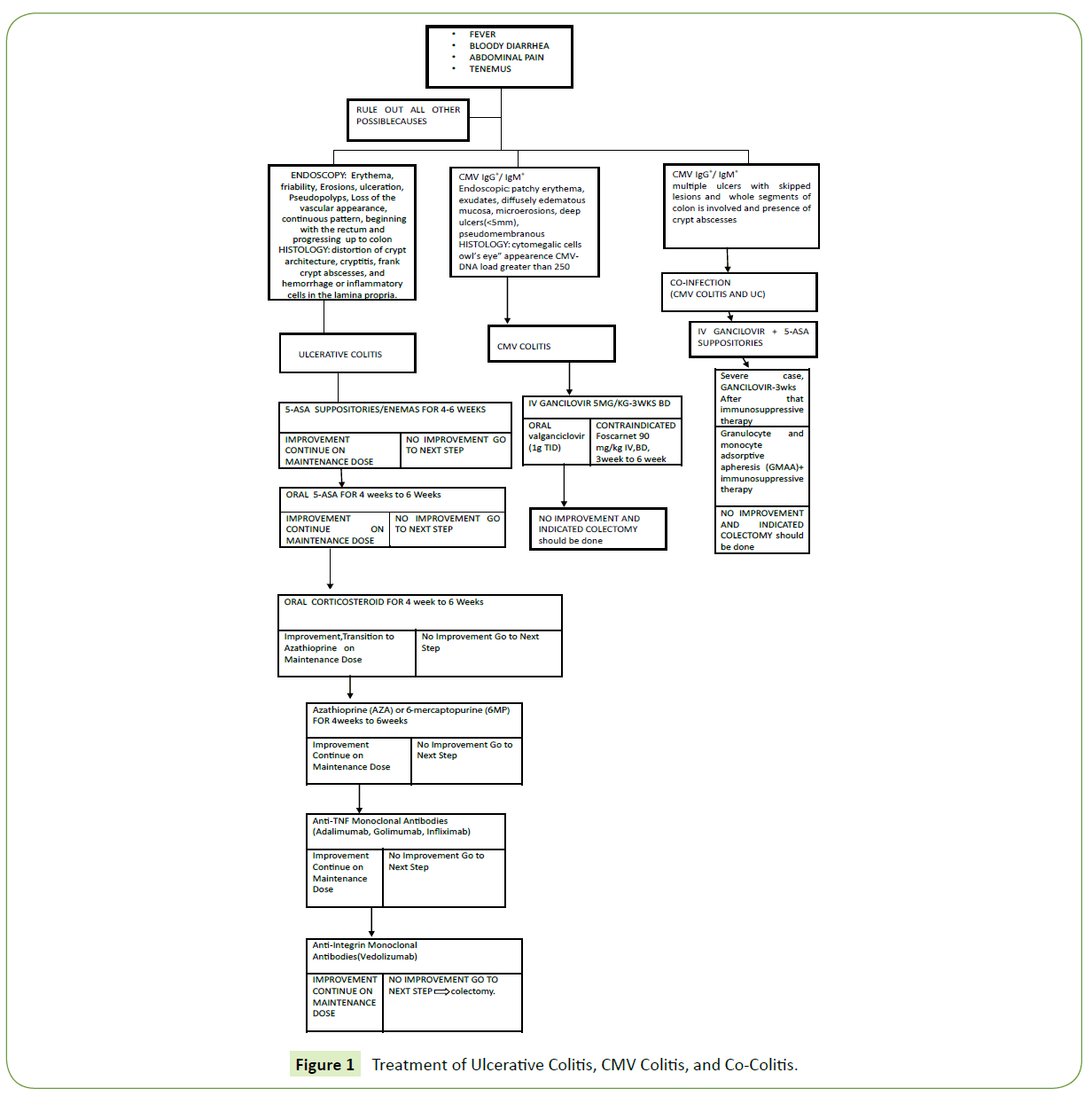
Ulcerative colitis, CMV colitis and co-colitis of UC and CMV colitis are similar in many aspects. The treatment of all these colitis is different including drugs, dose and the timing of starting the drugs. UC can be treated with immunosuppressive drugs while CMV colitis is treated with anti-viral drugs but Co-colitis if treated with immunosuppressive drugs can further deteriorate immunity letting virus to worsen its effect and diseases. So here we are comparing the treatment of all three colitis as shown in the Figure 1.
Ulcerative colitis (UC)
It is an immunologic disorder with unknown cause that results in inflammation and ulcers in the colon and rectum and it is a long term condition. It is a type of Inflammatory Bowel Disease (IBD) which is remitting and relapsing, in which inflammation is limited to mucosa and sub-mucosa of the colon and rectum sparing the upper GI tract. Symptoms consist of frequent loose bloody stools, cramps and weight loss. The typical histological finding of UC is crypt abscess, decrease number of goblet cells, distortion of mucosal glands, and inflammation of mucosa, polymorph nuclear leukocytes, and mononuclear cells.
The treatment of choice for mild to moderate UC is topical 5-aminosalicylic acid (5-ASA), which can be rectally applied as suppositories or enemas. 5-aminosalicylic acid has greater than 90% remission and mesalamine enemas have more than 93% remission rates, in 75% cases they can maintain remission [72- 78]. Topical 5-aminosalicylic acid have rapid action compared to oral and do not need repeat dosing [79]. 5-aminosalicylic acid in enema preparations can reach up to proximal sigmoid colon and splenic flexure, while foam form reaches up to middle of sigmoid colon and the suppositories reaches (5 cm to 8 cm) of the distal rectum [80,81]. 5-aminosalicylic acid is superior to corticosteroids in induction of remission, lower side effect and cheaper price [82,83]. The detail dosing and duration of 5-ASA is described in Figure 1.
When there is no remission with oral or topical 5-ASA than it can be combined with steroids, even if there is no response within 2weeks to 4 weeks than before giving glucocorticoid Budesonide- multimatrix can be used.Two separate studies show that budesonide has higher remission rate and less complication compared to steroids [84,85]. In severe UC cases where patients fail to recover with budesonides than glucocorticoid can be given. Oral glucocorticoid is very effective in active UC [13]. Cyclosporine can be used for severe UC for short duration in patients who did not respond to glucocorticoid since it is ineffective and unsafe for longer use [86,87], for the severe UC patients who needed longer duration treatment, long acting azathioprine (AZA) or 6-mercaptopurine can be given. For the patients who fail to AZA or 6-MP, Infliximab is another alternative, which has quicker remission and better maintenance rate [88]. Colectomy is done to all those severe UC who fail to response to cyclosporine and infliximab.
Treatment of CMV colitis
Immune-competent patients are asymptomatic after the primary infection, so most of them are unaware that they have been infected. Acute CMV infection manifests itself symptoms similar to mononucleosis such as muscle pain, fever, sore throat, enlarge lymph node, atypical lymphocytes and absolute lymphocytosis [21]. There is no cure for CMV disease in the latent state and infection will persist asymptomatically.
In immune-compromised patients it is very difficult to differentiate between UC and CMV colitis since both the disease can have extra-intestinal symptoms. CMV colitis is the second only to CMV retinitis that is commonly affected with CMV. In immune-compromised patients CMV colitis is due to the reactivation of the latent infection but in Immune-competent patients it can even occur in primary infection as severe CMV colitis. One study reported that 7 out of 15 immune-competent adults with CMV colitis had primary CMV infection [89].
The treatment of CMV infection weather it is primary or secondary infection is antiviral therapy.CMV colitis is also treated with antiviral drugs as other CMV infection. Ganciclovir is the most commonly used antiviral drugs. The other available antiviral drugs are foscarnet, valganciclovir and cidofovir [90- 92]. Ganciclovir is given 5mg/kg two times a day for three weeks intravenously because it has a poor oral bioavailability [90-92]. When the condition of patient become better than, patient can take oral ganciclovir(1g--tid). The side effects of this drug is neutropenia, bone marrow suppression, rash, headache, fever, somnolence, psychosis, high transaminases [90]. Foscarnet (90mg/kg—IV—BID—for 3weeks to 6 weeks) can be used when ganciclovir is contraindicated [92]. Foscarnet main side effect is nephrotoxicity. The rate of remission after antiviral treatment in IBD patients with CMV colitis is (67-100)% [93-96].
Co-Colitis (Cmv colitis and Ulcerative colitis)
The first case of co-colitis was reported in 1990 [97], since then many cases have been reported. The incidence of co- colitis is due to reactivation of latent viral infection are 15.8% to 34% [98], particularly in the severe UC, corticosteroid refractory and corticosteroid dependent patients who are treated with immunosuppressive such as cyclosporine, azathioprine and methotrexate, either alone or in combination [99,100]. One study from Japan reported a case report of co-colitis in a patient treated with leukocytapheresis (LCAP) therapy for UC [101]. From 1990 to 2013, 16 cases of co-colitis have been reported by ten authors [97,102-110]. CMV infection in these co-colitis were primary rather than reactivation of it. These study shows that co-colitis may be due to primary infection or due to reactivation of latent infection.The symptoms and sign of co-colitis are Fever and diarrhea in 88.2% patients, 47.1% patients’ has abdominal pain, 52.9% has Leukocytosis, 41.2% has abnormal liver function and 35.3% has an atypical lymphocytosis [107].
The majority of co-colitis is missed in newly diagnosed UC patients in routine clinical practice. The blood and serology test can be negative in active CMV colitis, which can delay the timely diagnosis of CMV colitis. The typical endoscopic finding of co-colitis is multiple ulcers with skipped lesions, trans-mural and presence of crypt abscesses; pseudo membrane may or may not be present [111-115]. Colonoscopy and biopsy helps in the diagnosis and assessing the severity of disease. Sensitivity of test is increased with immune-histochemistry use [116].
In immune mediated diseases such as co-colitis, it is very difficult to balance between decreasing immune suppression to allow antiviral immune responses to develop and increasing immune suppression to suppress the underlying disease process so the treatment of co-colitis vary in the different study. Crowley B, et al. in their study among ten patients with co-colitis, 4 needed only antiviral therapies, and another 4 patients needed only immune suppression and 2 needed both antiviral and immune suppression for improvement [117]. Vega R, et al in their study of 9 patients showed clinical improvement with antiviral drugs and stopping immunosuprresors [118]. An article from Japan shows that eight patients among the twelve patients with co-colitis respond only to anitiviral drugs [119]. In another study, it was found that 3 out of 7 co-colitis cases responded to UC treatment alone [120].
Prior to the use of gancilovir in co-colitis, surgery was needed in 80% patients and death rate was 33% [121]. Co-colitis patients needed higher surgical intervention compared to UC alone as one study shows (40:8)% [122]. So timely treatment with anti-viral drugs and anti-inflammatory drugs may be advantageous.
As different study shows different mode of treatment, it might be wise to treat patient with oral antiviral and topical 5-ASA in mild to moderate case. In severe cases, CMV should be cleared before starting conventional anti-inflammatory treatment or other immunosuppressive therapy.
Conclusion
Cytomegalovirus sometimes is a contributor and sometimes just a bystander. The Ulcerative Colitis, CMV colitis and co-colitis are symptomatically and endoscopically similar. So the early diagnosis and treatment of these colitis can decrease the need of colectomy and mortality rate. Ulcerative Colitis is treated with immunosuppressive drugs, and CMV colitis is treated with antiviral drugs while co-colitis should be treated with antiviral first followed by immunosuppressive. In co-colitis early clearing of virus makes immunosuppressive more effective and less side effect.
Disclosure
There is No any financial tie to disclose. No any authors have any conflict of interest for this review.
References
- Taylor GH (2003) Cytomegalovirus. Am Fam Physician 67(3): 519-526.
- Lockwood MR, Liddle J, Kitsanta P (2006) Cytomegalovirus colitis – an unusual cause for diarrhoea in an elderly woman. Age Ageing 35: 198-200.
- Dieterich DT, Rahmin M (1991) Cytomegalovirus colitis in AIDS: presentation in 44 patients and a review of the literature. J Acquir Immune Defic Syndr 4(Suppl. 1): S29-35.
- Yoshikawa T (2003) Significance of human herpes viruses to transplant recipients. Curr Opin Infect Dis 16: 601-606.
- Powell RD, Warner NE, Levine RS (1961) Cytomegalic inclusion disease and ulcerative colitis: Report of a case in a young adult. Am J Med 30: 334-340.
- Rowe WP, Hartley JW, Waterman S (1956)Cytopathogenic agent resembling human salivary gland virus recovered from tissue cultures of human adenoids. Proc Soc Exp Biol Med. 92: 418-424.
- Smith MG (1956) Propagation in tissue cultures of a cytopathogenic virus from human salivary gland virus (SGV) disease. Proc Soc Exp Biol Med 92: 424-430.a
- Weller TH, Macauley JC, Craig JM (1957) Isolation of intranuclear inclusion producing agents from infants with illnesses resembling cytomegalic inclusion disease. ProcSocExpBiol Med 94: 4-12.
- Weller TH, Hanshaw JB, Scott DE (1960) Serologic differentiation of viruses responsible for cytomegalic inclusion disease. Virology 12: 130-132.
- Pfau P, Kochman ML, Furth E, Lichtenstein GR (2001) Cytomegalovirus colitis complicating ulcerative colitis in the steroid-naïve patient. Am J Gastroenterol96: 895-899.
- Klemola E, Kääriäinen L (1965) Cytomegalovirus as a possible cause of a disease resembling infectious mononucleosis. Br Med J 2:1099.
- Staras SA, Dollard SC, Radford KW (2006) Seroprevalence of cytomegalovirus infection in the United States. Clin Infect Dis 43:1143.
- Ho M (1990) Epidemiology of cytomegalovirus infections. Rev Infect Dis 12 Suppl 7:S701.
- Bate SL, Dollard SC, Cannon MJ (2010) Cytomegalovirus seroprevalence in the United States: the national health and nutrition examination surveys. Clin Infect Dis 50:1439.
- Kim JJ, Simpson N, Klipfel N, Debose, Barr N, et al. (2010) Cytomegalovirusinfection in patients with active inflammatory bowel disease. Dig Dis Sci 55: 1059-1065.
- Kambham N, Vij R, Cartwright CA, Longacre T(2004) Cytomegalovirus infectionin steroid-refractory ulcerative colitis: a case-control study. Am J Surg Pathol 28: 365-373.
- Maconi G, Colombo E, Zerbi P (2005) Prevalence, detection rate and outcome of cytomegalovirus infection in ulcerative colitis patients requiring colonic resection. Dig Liver Dis 37(6):418-423.
- Kim YS, Kim YH, Kim JS (2012) for the IBD Study Group of the Korean Association for the Study of Intestinal Diseases(KASID), Korea, Cytomegalovirus infection in patients with new onset ulcerative colitis: a prospective study. Hepatogastroenterology 59(116):1098-101.
- Gronborg HL, Jespersen S, Honge BL, Jensen-Fangel S, Wejse C (2017) Review of cytomegalovirus co infection in HIV-infected individuals in Africa. Rev Med Virol 27(1).
- Sager K, Alam S, Bond A, Chinnappan L, Probert CS (2015) Review article: cytomegalovirus and inflammatory bowel disease. Aliment Pharmacol Ther 41(8):725-733.
- Evans AS (1978) Infectious mononucleosis and related syndromes. Am J Med Sci 276:325.
- Handsfield HH, Chandler SH, Caine VA, et al. (1985) Cytomegalovirus infection in sex partners: evidence for sexual transmission. J Infect Dis 151:344.
- Jordan MC, Rousseau WE, Noble GR, et al. (1973) Association of cervical cytomegaloviruses with venereal disease. N Engl J Med 288:932.
- Pass RF, Little EA, Stagno S (1987) Young children as a probable source of maternal and congenital cytomegalovirus infection. N Engl J Med 316:1366.
- Adler SP (1988) Molecular epidemiology of cytomegalovirus: viral transmission among children attending a day care center, their parents, and caretakers. J Pediatr 112:366.
- Ko JH, Peck KR, Lee WJ (2015) Clinical presentation and risk factors for cytomegalovirus colitis in immuno competent adult patients. Clin Infect Dis 60:e20.
- Tolpin MD, Stewart JA, Warren D (2015) Transfusion transmission of cytomegalovirus confirmed by restriction endonuclease analysis. J Pediatr 107:953.
- Prince AM, Szmuness W, Millian SJ, David DS (1985) A serologic study of cytomegalovirus infections associated with blood transfusions. N Engl J Med 284:1125.
- Yoshikawa T (2003) Significance of human herpesviruses to transplant recipients. CurrOpin Infect Dis 16: 601-606.
- Pass RF (1985) Epidemiology and transmission of cytomegalovirus. J Infect Dis 152:243-248.
- Plosa EJ, Esbenshade JC, Fuller MP (2012) Cytomegalovirus infection. Pediatr Rev 33:156-163.
- Stowell JD, Forlin-Passoni D, Din E (2012) Cytomegalovirus survival on common environmental surfaces: opportunities for viral transmission. J Infect Dis 205:211.
- Jean F, Thomas L, Molloy SS, Liu G, Jarvis MA, et al.(2000) A protein-based therapeutic for human cytomegalovirus infection. Proc Natl Acad Sci USA 97: 2864-2869.
- Nakayama K (1997) Furin, a subtilisin/Kex2p-like pro-protein convertase. Biochem J 327[Pt3]: 625-635.
- Miller-Kittrell M, Sparer TE (2009) Feeling manipulated: cytomegalovirus immune manipulation. Virol J 6:4.
- Froberg MK (2004) Review: CMV escapes! Ann Clin Lab Sci34:123-130.
- Hengel H, Brune W, Koszinowski UH (1998) Immune evasion by cytomegalovirus—survival strategies of a highly adapted opportunist. Trends Microbiol 6:190-197.
- Michelson S (1999) Human cytomegalovirus escapes from immune detection. Intervirology 42: 301-307.
- Rubin R, Gilman M, Kradin R (2006) Case 1-2006: A 64 year-old male lung-transplant recipient with fever, cough, hemoptysis and abdominal pain, N Engl J Med 354:180-187.
- De la H oz R E, Stephens G, Sherlock C (2002) Diagnosis and treatmentapproaches of CMV infections in adult patients. J ClinVirol 25(suppl 2):S1-12.
- Whitley R J, Jacobson MA, Friedberg DN, et al.(1998) Guidelines for the treatment of cytomegalovirus diseases in patients with AIDS in the era of potent antiretroviral therapy: Recommendations of an international panel, International AIDS Society, USA. Arch Intern Med 158:957-969.
- Papadakis KA, Tung JK, Binder SW (2001) Outcome of cytomegalovirus infections in patients with inflammatory bowel disease. Am J Gastroenterol 96:2137–2142.
- Kishore J, Ghoshal U, Ghoshal UC (2004) Infection with cytomegalovirusin patients with inflammatory bowel disease: Prevalence, clinical significance and outcome. J Med Microbiol 53:1155-1160.
- Ginsburg CH, Dambrauskas JT, Ault KA (1983) Impaired naturalkiller cell activity in patients with inflammatory bowel disease: Evidence for a qualitative defect. Gastroenterology 85:846-851.
- Pereyra F, Rubin RH (2004) Prevention and treatment of cytomegalovirusinfection in solid organ transplant recipients. Curr Opin Infect Dis 17:357-361.
- Waldman WJ, Adams PW, Orosz CG, et al.(1992) T lymphocyte activationby cytomegalovirus-infected, allogeneic cultured human endothelial cells. Transplantation 54:887-896.
- Hommes D, Sterringa G, J.H. van Deventer S, et al.(2004) The pathogenicity of cytomegalovirus in inflammatory bowel disease. Inflamm Bowel Dis 10:245-250.
- Fuss IJ, Neurath M, Boirivant M (1996) Disparate CD4+ lamina propria (LP) lymphokine secretion profiles in inflammatory bowel disease, Crohn’s disease LP cells manifest increased secretion of IFN-gamma, whereas ulcerative colitis LP cells manifest increased secretion of IL-5. J Immunol 157:1261-1270.
- Strober W, Fuss IJ (2011) Proinflammatory cytokines in the pathogenesis of inflammatory bowel diseases. Gastroenterology 140:1756-1767.
- Goodgame RW (1993) Gastrointestinal cytomegalovirus disease. Ann Intern Med 119: 924-935.
- Klauber E, Briski LE, Khatib R (1998) Cytomegalovirus colitis in the immuno competent host: an overview, Scand J Infect Dis 30: 559-564.
- Ho M(1977) Virus infections after transplantation in man, Brief review. Arch Virol 55: 1-24.
- Lawlor G, Moss AC (2010)Cytomegalovirus in inflammatory bowel disease: pathogen or innocent bystander? Inflamm Bowel Dis 16: 1620-1627.
- Domènech E, Vega R, Ojanguren I, Hernández A, Garcia-Planella, et al. (2008) Cytomegalovirus infection in ulcerative colitis: a prospective, comparative study on prevalence and diagnostic strategy. Inflamm Bowel Dis 14: 1373-1379.
- Kandiel A, Lashner B (2006) Cytomegalovirus colitis complicating inflammatory bowel disease, Am J Gastroenterol 101:2857-2865
- Garrido E, Carrera E, Manzano R, Lopez-Sanroman A (2013)Clinical significance of cytomegalovirus infection in patients with inflammatory bowel disease. World J Gastroenterol 19: 17-25.
- Ljungman P, Griffiths P, Paya C (2002) Definitions of cytomegalovirus infection and disease in transplant recipients. Clin Infect Dis 34(8):1094-1097.
- Domènech E, Vega R, Ojanguren I, Hernández A, Garcia- Planella E, et al. (2008) Cytomegalovirus infection in ulcerative colitis: a prospective, comparative study on prevalence and diagnostic strategy. Inflamm Bowel Dis 14: 1373-1379.
- Boivin G, Handfield J, Toma E, Murray G, Lalonde R, et al. (1998) Evaluation of the AMPLICOR cytomegalovirus test with specimens from human immunodeficiency virus-infected subjects. J Clin Microbiol 36: 2509-2513.
- Criscuoli V, Rizzuto MR, Cottone M (2006) Cytomegalovirus and inflammatory bowel disease: is there a link?. World J Gastroenterol 12: 4813-4818.
- Matsuoka K, Iwao Y, Mori T, Sakuraba A, Yajima T(2007) Cytomegalovirus is frequently reactivated and disappears without antiviral agents in ulcerative colitis patients. Am J Gastroenterol 102: 331-337.
- Nakase H, Matsumura K, Yoshino T, Chiba T (2008) Systematic review: cytomegalovirus infection in inflammatory bowel disease. J Gastroenterol 43: 735-740.
- Michaelides A, Liolios L, Glare EM, Spelman DW, Bailey MJ,et al.(2001) Increased human cytomegalovirus (HCMV) DNA load in peripheral blood leukocytes after lung transplantation correlates with HCMV pneumonitis. Transplantation 72: 141-147.
- Rowshani AT, Bemelman FJ, van Leeuwen EM, van Lier RA, ten Berge IJ (2005) Clinical and immunologic aspects of cytomegalovirus infection in solid organ transplant recipients. Transplantation 79: 381-386.
- Gerna G, Lilleri D (2006) Monitoring transplant patients for human cytomegalovirus: Diagnostic update. Herpes 13: 4-11.
- Boom R, Sol C, Weel J, Lettinga K, Gerrits Y, et al. (2000) Detection and quantitation of human cytomegalovirus DNA in faeces. J Virol Methods 84: 1-14.
- Beaugerie L, Cywiner-Golenzer C, Monfort L,et al.(1997) Definition and diagnosis of cytomegalovirus colitis in patients infected by human immunodeficiency virus. J Acquir Immune Defic Syndr Hum Retrovirol 14:423-429.
- Roblin X, Pillet S, Oussalah A, Berthelot P, Del Tedesco E, et al. (2011) Cytomegalovirus load in inflamed intestinal tissue is predictive of resistance to immunosuppressive therapy in ulcerative colitis. Am J Gastroenterol 106: 2001-2008.
- Smail Hakk1, KALKAN1, Ulku DA⁄LI2 (2010)What is the most accurate method for the diagnosis of cytomegalovirus (CMV) enteritis or colitis?.Turk J Gastroenterol 21(1): 83-86.
- Streetz KL, Buhr T,Wedemeyer H, et al.(2003) Acute CMV-colitis in a patient with a history of ulcerative colitis. Scand J Gastroenterol 38:119-122.
- Papadakis KA, Tung JK, Binder SW,et al.(2001) Outcome of cytomegalovirus infections in patients with inflammatory bowel disease. Am J Gastroenterol 96:2137-2142.
- Hanauer SB (1996) Inflammatory bowel disease. N Engl J Med 334:841.
- Biddle WL, Greenberger NJ, Swan JT (1988) 5-Aminosalicylic acid enemas: effective agent in maintaining remission in left-sided ulcerative colitis. Gastroenterology 94:1075.
- Campieri M, Lanfranchi GA, Bazzocchi G (1981) Treatment of ulcerative colitis with high-dose 5-aminosalicylic acid enemas. Lancet 2:270.
- Campieri M, De Franchis R, Bianchi Porro G (1990) Mesalazine (5-aminosalicylic acid) suppositories in the treatment of ulcerative proctitis or distal proctosigmoiditis, A randomized controlled trial. Scand J Gastroenterol 25:663.
- Friedman LS, Richter JM, Kirkham SE, et al.(1986) 5-Aminosalicylic acid enemas in refractory distal ulcerative colitis: a randomized, controlled trial. Am J Gastroenterol 81:412.
- Marshall JK, Irvine EJ (1995) Rectalaminosalicylate therapy for distal ulcerative colitis: a meta-analysis. Aliment PharmacolTher 9:293.
- Kam L, Cohen H, Dooley C, et al. (1996) A comparison of mesalamine suspension enema and oral sulfasalazine for treatment of active distal ulcerative colitis in adults. Am J Gastroenterol 91:1338.
- Kornbluth A, Sachar DB (2010) Practice Parameters Committee of the American College of Gastroenterology, Ulcerative colitis practice guidelines in adults: American College Of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol 105:501.
- Chapman NJ, Brown ML, Phillips SF, et al.(1992) Distribution of mesalamine enemas in patients with active distal ulcerative colitis. Mayo ClinProc 67:245.
- Farthing MJ, Rutland MD, Clark ML (1979) Retrograde spread of ydrocortisone containing foam given intrarectally in ulcerative colitis. Br Med J. 2:822.
- Marshall JK, Irvine EJ (1997)Rectal corticosteroids versus alternative treatments in ulcerative colitis: a meta-analysis. Gut 40:775.
- Cohen RD, Woseth DM, Thisted RA, Hanauer SB (2000) A meta-analysis and overview of the literature on treatment options for left-sided ulcerative colitis and ulcerative proctitis. Am J Gastroenterol 95:1263.
- Sandborn WJ, Travis S, Moro L, et al. (2012) Once-daily budesonide MMX® extended-release tablets induce remission in patients with mild to moderate ulcerative colitis: results from the CORE I study. Gastroenterology 143:1218.
- Travis SP, Danese S, Kupcinskas L, et al. (2014) Once-daily budesonide MMX in active, mild-to-moderate ulcerative colitis: results from the randomised CORE II study. Gut 63:433.
- Moskovitz DN, Van Assche G, Maenhout B, et al. (2006) Incidence of colectomy during long-term follow-up after cyclosporine-induced remission of severe ulcerative colitis.ClinGastroenterolHepatol 4:760.
- Cohen RD (2009)How should we treat severe acute steroid-refractory ulcerative colitis?.Inflamm Bowel Dis 15:150.
- Järnerot G, Hertervig E, Friis-Liby I, et al. (2005) Infliximab as rescue therapy in severe to moderately severe ulcerative colitis: a randomized, placebo-controlled study. Gastroenterology 128:1805.
- Klauber E, Briski LE, Khatib R (1998) Cytomegalovirus colitis in the immunocompetent host: an overview.Scand J Infect Dis 30: 559– 564.
- Faulds D, Heel RC, Ganciclovir (1990) A review of its antiviral activity, pharmacokinetic properties and therapeutic efficacy in cytomegalovirus infections. Drugs 39: 597-638.
- Markham A, Faulds D, Ganciclovir (1994)An update of its therapeutic use in cytomegalovirus infection. Drugs 48: 455-484.
- Heuman DM (2019) Cytomegalovirus colitis. Medscape.
- Criscuoli V, Casa A, Orlando A, et al.(2004) Severe acute colitis associated with CMV: A prevalence study. Dig Liver Dis 36:818–820.
- Cottone M, Pietrosi G, Martorana G, et al. (2001) Prevalence of cytomegalovirus infection in severe refractory ulcerative and Crohn’s colitis. Am J Gastroenterol 96:773–775.
- Papadakis KA, Tung JK, Binder SW, et al. (2001) Outcome of cytomegalovirus infections in patients with inflammatory bowel disease. Am J Gastroenterol 96:2137–2142.
- Vega R , Bertran X, Menacho M, et al. (1999) Cytomegalovirus infection in patients with inflammatory bowel disease. Am J Gastroenterol94:1053–1056.
- Diepersloot RJ, Kroes AC, Visser W, Jiwa NM, Rothbarth PH(1990) Acute ulcerative proctocolitis associated with primary cytomegalovirus infection.ArchIntern Med 150:1749–1751.
- Papadakis KA, Tung JK, Binder SW, et al.(2001) Outcome of cytomegalovirusinfections in patients with inflammatory bowel disease.Am J Gastroenterol 96: 2137-2142.
- Summers RW(2007) Novel and future medical management of inflammatorybowel disease.SurgClin North Am 87: 727-741.
- Clark M, Colombel JF, Feagan BC, et al. (2007)American gastroenterologicalassociation consensus development conference on the use of biologics in the treatment of inflammatory bowel disease. Gastroenterology 133: 312-339.
- Rie Osaki, Akira Andoh, TomoyukiTsujikawa et al. (2008) Acute Cytomegalovirus Infection Superimposed on Corticosteroid-Naive Ulcerative Colitis. Inter Med 47: 1341-1344.
- Lortholary O, Perronne C, Leport J, Leport C, Vilde JL(1993)Primary cytomegalovirus infection associated with the onset of ulcerative colitis.Eur J ClinMicrobiol Infect Dis 12:750–752.
- Orvar K, Murray J, Carmen J, Conklin J (1993) Cytomegalovirus infection associated with onset of inflammatory bowel disease. Dig Dis Sci38:2307–2310.
- Mate Del Tio M, de Rivera JM PS, LarrauriMartinez J, Garces Jimenez MC,Barbado Hernandez FJ (1996) Association of cytomegalovirus colitis and the 1stepisode of ulcerative colitis in an immunocompetent patient. GastroenterolHepatol 19:206–207.
- Aoyagi K, Kanamoto K, Koga H, Nakamura S, Hirakawa K, et al. (1998) Cytomegalovirus infection complicating ulcerative colitis, Stomach and Intestine, Tokyo 33:1261–1265.
- Hussein K, Hayek T, Yassin K, Fischer D, Vlodavsky E, et al.(2006) Acute cytomegalovirus infection associated with the onset of inflammatory bowel disease. Am J Med Sci 331:40–43.
- Martin SI, Sepehr A, Fishman JA (2006) Primary infection with cytomegalovirus in ulcerative colitis. Dig Dis Sci 51:2184–2187.
- Kim JJ, Simpson N, Klipfel N, Debose R, Barr N, et al. (2010) Cytomegalovirus infection in patients with active inflammatory bowel disease. Dig Dis Sci 55:1059–1065.
- Kim YS, Kim YH, Kim JS, Cheon JH, Ye BD, et al.(2012) IBD Study Group of the Korean Association for the Study of Intestinal Diseases (KASID), Korea: Cytomegalovirus infection in patients with new onset ulcerative colitis: a prospective study. Hepatogastroenterology 59:1098–1101.
- Chiba et al. (2013) Cytomegalovirus infection associated with onset of ulcerative colitis BMC Research Notes 6:40.
- Wilcox CM, Chalasani N, Lazenby A,Schwartz DA (1998) Cytomegalovirus colitis in acquired immunodeficiency syndrome: a clinical and endoscopic study. GastrointestEndosc 48:39–43.
- Lin WR, Su MY, Hsu CM, Ho YP, Ngan KW, et al. (2005) Clinical and endoscopic features for alimentary tract cytomegalovirus disease: reportof 20 cases with gastrointestinal cytomegalovirus disease. Chang GungMed J 28:476–484.
- Ng FH, Chau TN, Cheung TC, Kng C, Wong SY et al.(1999) Cytomegalovirus colitis in individuals withoutapparent cause of immunodeficiency. Dig Dis Sci 44:945–952.
- Battaglino MP,Rockey DC (1999) Cytomegalovirus colitis presenting with the endoscopic appearance of pseudo membranous colitis.GastrointestEndosc 50:697–700.
- Olofinlade O,Chiang C (2001) Cytomegalovirus infection as a cause of pseudomembrane colitis, a report of four cases. J Clinical Gastroenterol 32:82–84.
- . Kambham N, Vij R, Cartwright CA, Longacre T (2004)Cytomegalovirusinfection in steroid-refractory ulcerative colitis: a case-control study. Am J SurgPathol 28:365–373.
- Crowley B, Dempsey J, Olujohungbe A, Khan A, Mutton K,et al. (2002) Unusual manifestations of primary cytomegalovirus infection in patients without HIV infection and without organ transplants. J Med Virol 68:237–240.
- Vega R, Bertran X, Menacho M, Domenech E, Moreno de Vega V, HombradosMet al.(1999) Cytomegalovirus infection in patients with inflammatory bowel disease. Am J Gastroenterol 94:1053–1056.
- Wada Y, Matsui T, Matake H, Sakurai T, Yamamoto Jet al.(2003) Intractable ulcerative colitis caused by cytomegalovirus infection: a prospective study on prevalence, diagnosis, and treatment. Dis Colon Rectum 46(Suppl 10):S59–S65.
- Criscuoli V, Casa A, Orlando A, Pecoraro G, Oliva L et al.(2004) severe acute colitis associated with CMV: a prevalence study. Dig Liver Dis 36:818–820.
- Pfau P, Kochman ML, Furth E, Lichtenstein GR (2001)Cytomegalovirus colitis complicating ulcerative colitis in the steroidna ¨Ã±ve patient. Am J Gastroenterol 96:895–899.
- Kishore J, Ghoshal U, Ghoshal UC, Krishnani N, Kumar S, et al. (2004) Infection with cytomegalovirus in patients with inflammatory bowel disease: prevalence, clinical significance and outcome. J Med Microbiol 53:1155–1160.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences