Determinants of Adverse Pregnancy Outcomes among mothers who gave birth from Jan 1-Dec 31/2015 in Jimma University Specialized Hospital, Case control study, 2016
Eyosiyas Yeshialem, Nigus Alemnew, Mulumebet Abera and Amanuel Tesfay
DOI10.21767/2471-299X.1000063
Eyosiyas Yeshialem1*, Nigus Alemnew1, Mulumebet Abera2 and Amanuel Tesfay2
1Faculty of Public Health and Medical Science, Mettu University, Ethiopia
2Department of Population and Family Health, College of Public Health, Jimma University, Ethiopia
- *Corresponding Author:
- Eyosiyas Yeshialem
Faculty of Public Health and Medical Science
Mettu University
Oromia 231, Ethiopia
Tel: +251 913 836 869
E-mail: eyosi143@gmail.com
Received Date: December 14, 2017; Accepted Date: December 22, 2017; Published Date: December 29, 2017
Citation: Yeshialem E, Alemnew N, Abera M, Tesfay A (2017) Determinants of Adverse Pregnancy Outcomes among Mothers Who Gave Birth from Jan 1-Dec 31/2015 in Jimma University Specialized Hospital, Case Control Study, 2016. Med Clin Rev. 3:22. doi: 10.21767/2471-299X.1000063
Abstract
Background: Adverse pregnancy outcomes lead to serious health consequences to the mother and/or the baby. These Adverse birth outcomes; prematurity, low birth weight and still birth represent significant problems in both developing and developed countries. Adverse pregnancy outcomes are still major public health problems in developing countries including Ethiopia where most pregnancies are unplanned, complications are many and outcomes are generally Unfavorable for both mother and infant.
Objective: To identify determinants of adverse pregnancy outcomes among deliveries takes place in Jimma University specialized hospital from January 1 – December 31 / 2015.
Methods: The study was a facility based unmatched casecontrol study design conducted by reviewing mothers and newborn cards and registration log book who delivered in Jimma university specialized hospital from January 1 / 2015 to December 31/2015, southwest Ethiopia. The study was done on randomly selected 86 cases and 258 controls using structured data collection checklist. Data analysis was done by SPSS version 20 and multiple logistic regression statistical methods were used to identify the predictors.
Result: In this study 344 mothers and newborns cards were included yielding 100% response rate. From this 86 mothers and newborn cards were selected for case group and 258 mothers and newborn cards were selected for control group. Most of the cases 80.2% and controls 82.9% were between the age group of 20-34 years. Mothers who are referred for delivery service from other area are more than five times to have adverse pregnancy outcomes than mothers who are not referred, AOR=5.49 95% CI [2.80-10.76]. And mothers who had illness during current pregnancy are seven times to be case than controls, AOR=7.22, 95% CI [1.65-31.58]. Mothers who attend ante natal care (ANC) were 83% less likely to have adverse pregnancy outcome, than mothers who didn’t attended ANC follow up, AOR = 0.17 95% CI [0.06-0.49]. Pregnant mothers who are anemic or had hemoglobin level of less than 11 gram/dl are more than seven times to have adverse pregnancy outcomes than non-anemic pregnant mothers, AOR=7.29 95% CI [2.85-18.67]. Additionally, women who had obstetric emergencies during current pregnancy, complications during current delivery, and multiple pregnancy are more than 18 times AOR=18.40[6.12-55.37], 2 times AOR=2.65[1.38-5.11] and 7 times AOR=7.59[1.49-38.65] to have adverse pregnancy outcomes than their counterparts respectively.
Conclusion: According to the findings of this study; referral, illness during current pregnancy, having ANC attendance, anemia during current pregnancy, complication during delivery, multiple pregnancy and having obstetric emergencies are statistically significant predictors of adverse pregnancy outcomes.
Keywords
Anemia; Infant; Obstetric; Vaccination
Background
Pregnancy outcomes refer to life events that occur to the newborn infant from the age of viability (28 weeks) to the first week of life. The transition of fetus immersed in the amniotic fluid to life outside the womb is not always smooth and can result in adverse events to the mother or/and the baby. pregnancy outcomes varies from pregnancy to pregnancy which includes; normal live birth, low birth weight, prematurity in the baby, stillbirth, intrauterine fetal death, early neonatal death and late neonatal death. Adverse pregnancy outcomes are those pregnancy outcomes other than normal live birth which majorly includes preterm birth, stillbirth and low birth weight which are the major cause of neonatal morbidity, mortality and long term physical and psychological problems [1].
These Adverse birth outcomes; prematurity, low birth weight and still birth represent significant problems in both developing and developed countries. Each year, about 15 million babies in the world, more than one in 10 births, are born too prematurely. More than one million of those babies die shortly after birth; countless others suffer from lifelong physical, neurological, or educational disabilities, often at great cost to families and societies [2].
Among 136 million babies born every year, approximately 4 million are stillborn, and the other 4 million die in the first month of life. In 2006 Worldwide, 12% of babies are born prematurely, 8% with low birth weight, and 3% have major birth defects. Adverse pregnancy outcomes lead to serious health consequences to the mother and/or the baby [3].
This study was aimed to at assessing determinants of adverse pregnancy outcomes in Jimma university specialized hospital, Jimma town, Oromia regional state, Ethiopia.
Methods
Study area and period
The study was conducted in Jimma university specialized hospital. The hospital is one of the oldest public hospitals in the country located in Jimma town of Oromia Regional State, Ethiopia. The town is Located 357 km from Addis Ababa and JUSH is the only specialized teaching and referral hospital in the South Western region of Ethiopia.
The hospital has a predominantly rural catchment population of 15 million people for tertiary level care. According to 2006 fiscal year annual report, the hospital provided services for about 15,000 inpatient, 160,000 outpatient attendants, 11,000 emergency cases and around 5000 deliveries takes placed. The hospital has about 21 units and 503 beds where around 65 beds are found in Maternity ward. The ward has around 119 health professional and supportive staffs, namely: Seven (7) Senior Obstetricians and Gynecologists, 6 BSc Nurses, 6 BSc Midwives, 5 Diploma Nurses, 32 Diploma midwives,38 Residents, 16 Cleaners, 6 Porters and 3 Runners. The study was conducted from March 15- 30/ 2016.
Study design: Institution based case control study was conducted at JUSH in Jimma town, Oromia regional state.
Source population: All women who gave birth in JUSH from January 1, 2015 to December 31, 2015.
Study population
• For controls: selected women who gave normal live birth in JUSH from January 1, 2015 to December 31, 2015.
• For cases: selected women who gave birth with at least one adverse pregnancy outcome (preterm birth, stillbirth or low birth weight)in JUSH from January 1, 2015 to December 31, 2015.
Sampling unit: Mothers who gave normal birth for controls and mothers with at least one adverse pregnancy outcome (preterm, stillbirth, low birth weight) for cases were sampling units.
Inclusion criteria: All mothers who gave births from January 01/2015 December 30/2015 in JUSH were included.
Exclusion criteria: Mothers whose cards are missed and incomplete with outcome variable were excluded from the study.
Sample size determination
All recorded deliveries in the study period were included and Sample size was determined using the formula for two population proportion as follows.
Labor complication of last birth, complications during last pregnancy, residence (urban), Gravida (primi Gravida) and having ANC visit were considered in order to calculate required sample size by revising different literatures. To calculate sample size all the above exposure variables were considered and complication during current pregnancy was chosen as an independent variable since it gives maximum sample size as compared to other exposure variables (Table 1).
| Variables | Control% exposed/ AOR | Calculated sample size | ||
|---|---|---|---|---|
| Cases | Controls | Total | ||
| Complication during last labor-delivery | 3.5(9.94) | 26 | 78 | 104 |
| Complications during last pregnancy | 2.7(4.85) | 86 | 258 | 344 |
| Residence(urban) | 67.5(0.27) | 29 | 87 | 116 |
| Gravida (I) | 49(0.35) | 49 | 145 | 194 |
| Have ANC visit | 67.8(0.44) | 71 | 211 | 282 |
Table 1: Sample size calculation based on significant independent variables identified on literatures.
The sample size was calculated by (statistical EPI info 7.1.1) software package by considering that the percent of controls exposed among the controls is 2.7% (main exposure variable), with 4.85 odds ratio which is taken from similar study done in mekele town public hospitals, Ethiopia, 95% CI, 80% power of the study and case to control ratio of 1:3 [4].
Accordingly, the final sample size was 86 cases and 258 controls (a total sample size of 344) were involved in the study.
Sampling technique and data collection procedures
Simple random sampling technique was used with the following steps. A total of 1740 Births from 1st Jan to 31st Dec 2015 were identified using registration log book and 387 births were with at least one adverse pregnancy outcomes (LBW, preterm, stillbirth). Card number of identified births was coded for cases and controls. After the codes of cases and controls are entered in to SPSS version 20 software separately, 86 cases and 258 controls were selected randomly. Cards were traced and checked for completeness of the necessary information. Incomplete birth cards were excluded and replaced with another card.
The data was extracted from clinical records of mother’s and newborn’s (registration log books and individual cards) using a structured data collecting checklist. Selected mother’s cards on registration log book were traced through the hospital’s registry book. Structured checklist was prepared in English. The data was extracted by 2 diploma midwives &2 diploma nurses and two degree Midwives as supervisor. Training was given for reviewers and supervisor before actual data collection.
Data quality control and management
Data quality was ensured during collection, coding, entry and analysis. Structured checklist was used. Training was given to the reviewers and supervisors to avoid any confusion and have a common understanding about the study. Each card was checked for its consistency, provision of full information and appropriate documentation. Supervision of reviewers was done by supervisors. The reviewers were instructed to write cards number on the check list during the data collection so that any identified errors will be traced back using the cards number. The filled checklist was checked for completeness by reviewers, supervisors and PI on a daily basis. Consequently, any problem encountered was discussed among the team and solve immediately. Two days Training on method of reviewing, how to use the checklist and objective of the study was given for four data collectors and two supervisors.
Situational analysis
Situational analysis was conducted on 16 mother’s cards (taken as 5% of the total sample size) 4 cases and 12 controls in Shenen Gibie Hospital found in Jimma town before the actual data collection to control the quality of the tool.
Data processing and analysis
Collected Data was entered in to Epi Data version 3.1 and exported SPSS-version 20 for analysis.
Data was checked for consistency and completeness by exploratory data analysis before running the actual statistical analysis. Frequencies were used to see the overall distribution of the study subjects with regard to the variables under the study. Bivariate logistic regressions were used to select important variables candidate for the multiple logistic regression. Independent variables with p value less than 0.2 were selected as a candidate for multiple logistic regression. Finally, multiple logistic regression was used to assess the relative effect of independent variables on dependent variable and to control the possible confounders and finally to select important predictors of adverse pregnancy outcomes included in the model. Odds Ratio (OR) and their 95% Confidence Interval (CI) were used to measure the association. A significance level of 0.05 was used to decide the significance of statistical tests. Finally the results are presented in text, table and graphs.
Ethical considerations
Ethical clearance was obtained from Ethical review committee of college of health sciences, Jimma University to conduct the study. Further permission was obtained from Medical Director of Jimma university specialized hospital, department head of the obstetric ward and card room head for the utilization of logbooks and cards. Since the cards include the name of the mothers, confidentiality will be maintained by making the data collectors aware not to record any identification information found on the card.
Results
Socio-demographic characteristics of cases and controls
A total of 86 women (cases) and 258 controls were included in the study (Table 2). The mean age among the cases was 26.01 (± SD 5.49) years (range 18 to 40), and among the controls 25.34 (± SD 5.00) years (range 16 to 40). Additionally, 214(82.9%) of controls and 69 (80.2%) of cases are within the age group of 20-34 years. In addition, 134 (51.9%) of the controls and 32 (37.2%) of the cases are Gravida one. With regards to the participants residence, majority of cases 58 (67.4%) and only 84 (32.6%) controls are rural in residents.
| Controls /n=258 N (%) | Cases n=86 N (%) | Total N=344 N (%) | ||
|---|---|---|---|---|
| Age | 15-19 years | 21(8.1) | 6(7.0) | 27(7.8) |
| 20-34 years | 214(82.9) | 69(80.2) | 283(82.3) | |
| 35 and above | 23(8.9) | 11(12.8) | 34(9.9) | |
| Gravidity | One | 134(51.9) | 32(37.2) | 166(48.3) |
| 02-Apr | 111(43.0) | 43(50.0) | 154(44.8) | |
| Five and more | 13(5.0) | 11(12.8) | 24(7.0) | |
| Residence of mothers | Urban | 174(67.4) | 28(32.6) | 202(58.7) |
| Rural | 84(32.6) | 58(67.4) | 142(41.3) | |
Table 2: Socio-demographic characteristics of the cases and controls, at Jimma University specialized hospital, Jimma, Ethiopia, 2015.
Past obstetric and gynecologic characteristics of cases and controls
This study shows that 1(0.4%) of the controls and 3(3.5%) of the cases had a recorded complication in their previous pregnancies. Additionally 15(5.8%) controls and 14 (16.3%) cases had history of abortion while 11(4.3%) of controls and 12(14.0%) cases had previous adverse pregnancy outcomes (Table 3).
| Controls/ n=258 N (%) | Cases / n=86 N (%) | Total / N=344 N (%) | |||||
|---|---|---|---|---|---|---|---|
| Any obstetric complications in previous pregnancy? | No | 257 | -99.6 | 83 | -96.5 | 340 | -98.8 |
| Yes | 1 | -0.4 | 3 | -3.5 | 4 | -1.2 | |
| Any history of abortion? | No | 243 | -94.2 | 72 | -83.7 | 315 | -91.6 |
| Yes | 15 | -5.8 | 14 | -16.3 | 29 | -8.4 | |
| Previous History of Adverse pregnancy outcomes | No | 247 | -95.7 | 74 | -86 | 321 | -93.3 |
| Yes | 11 | -4.3 | 12 | -14 | 23 | -6.7 | |
| Ever used family planning methods? | No | 96 | -37.2 | 35 | -40.7 | 131 | -38.1 |
| Yes | 162 | -62.8 | 51 | -59.3 | 213 | -61.9 | |
| Type of modern family planning methods used | Pills & injectable | 145 | -56.2 | 42 | -48.9 | 187 | -54.4 |
| Implants | 15 | -5.8 | 4 | -4.7 | 19 | -5.5 | |
Table 3: Past obstetric and gynecologic characteristics of the cases and controls, at JUSH, Jimma, Ethiopia, 2015.
The study also indicates that 162(62.8%) of controls and 51(59.3%) of the cases ever used modern family planning methods where majority of controls 145(56.2%) and cases 42(48.9%) used pills & injectable family planning methods.
The study also indicates that, Six (2.33%) of controls had previous history of early neonatal death while five (5.81%) of cases had previous history of stillbirth and low birth weight each.
Previous and current medical characteristics of cases and controls
The result of this study shows that 4(1.6%) of the controls and 8(9.3%) of cases had record of pre-existing medical illness where 5(5.81) of cases experience hypertension. Four (1.6%) of controls and 12(14.0%) of cases had medical illness during their current pregnancy (Table 4). Concerning HIV/AIDS, 253(98.1%) of controls and 86(100%) of cases are tested for HIV/AIDS where 251(99.2%) of controls and 85(98.8%) of cases are non-reactive and all the reactive mothers among both group are on anti- retroviral treatment (ART). Additionally, Nine (3.5%) of control and 27(31.4%) of cases had been diagnosed as having anemia during their current pregnancy.
| Characteristics | Controls/ n=258 Count (%) | Cases/ n=86 Count (%) | Total/ N=344 Count (%) | |
|---|---|---|---|---|
| pre-existing medical illness | No | 254(98.4) | 78(90.7) | 332(96.5) |
| Yes | 4(1.6) | 8(9.3) | 12(3.5) | |
| Illnesses during current pregnancy | No | 254(98.4) | 74(86.0) | 328(95.3) |
| Yes | 4(1.6) | 12(14.0) | 16(4.7) | |
| HIV test status | Tested | 253(98.1) | 86 (100.0) | 339 (98.5) |
| HIV test result | Non-reactive | 251(99.2) | 85 (98.8) | 336 (99.1) |
| Reactive | 2(.8) | 1(1.2) | 3 (0.9) | |
| Anemia status | Non anemic | 249 (96.5) | 59 (68.6) | 308 (89.5) |
| Anemic | 9 (3.5) | 27 (31.4) | 36 (10.5) | |
Table 4: Distribution of previous and current medical illnesses among cases and controls, at Jimma University specialized hospital, Jimma, Ethiopia, 2015.
Current Obstetric characteristics of cases and controls
Majority of the controls, 243(94.2%) and 75(87.2%) cases had planned pregnancy. The proportion of women who received at least one ANC service was higher among controls 246(95.3%) than cases 68 (79.1%) where 173(67.1%) and 31 (36.0%) of controls and cases had ANC visit of four and above respectively (Table 5).
| characteristics | Controls/N=258 | Cases N=86 | Total/N=344 | ||||
|---|---|---|---|---|---|---|---|
| Count | % | Count | % | Count | % | ||
| pregnancy status | planned | 243 | 94.2 | 75 | 87.2 | 318 | 92.4 |
| unplanned | 14 | 5.4 | 11 | 12.8 | 25 | 7.3 | |
| ANC follow-up | no | 11 | 4.3 | 17 | 19.8 | 28 | 8.1 |
| yes | 247 | 95.7 | 69 | 80.2 | 316 | 98.9 | |
| Frequency of ANC visits | 1 visit | 2 | 0.8 | 3 | 3.5 | 5 | 1.5 |
| 2 -3 visits | 72 | 27.9 | 35 | 40.7 | 107 | 31.1 | |
| 4 and more visits | 173 | 67.1 | 31 | 36 | 204 | 59.3 | |
| TT vaccination status | no | 12 | 4.7 | 21 | 24.4 | 33 | 9.6 |
| yes | 154 | 59.7 | 43 | 50 | 197 | 57.3 | |
| not recorded | 92 | 35.7 | 22 | 25.6 | 114 | 33.1 | |
| Any Medication taken during current pregnancy | no | 256 | 99.2 | 83 | 96.5 | 339 | 98.5 |
| yes | 2 | 0.8 | 3 | 3.5 | 5 | 1.5 | |
| Obstetric emergencies at current pregnancy | no | 252 | 97.7 | 67 | 77.9 | 319 | 92.7 |
| yes | 6 | 2.3 | 19 | 22.1 | 25 | 7.3 | |
Table 5: Current Obstetric characteristics of cases and controls, at Jimma University specialized hospital, Jimma, Ethiopia, 2015.
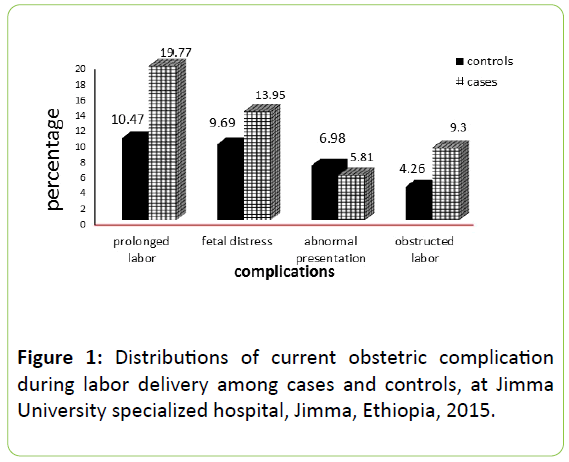
Having at least one Tetanus toxoid vaccination was slightly lower among cases (50.0%) compared to (59.7%) controls that have got tetanus vaccination during current pregnancy. Higher proportions of cases 19(22.1%) than controls 6 (2.3%) had at least one obstetric emergency during their current pregnancy (Figure 1).
This study investigated that, Stillbirth comprises majority of adverse birth outcomes contributing 62.7% of cases while low birth weight and Preterm birth take second and third respectively (Table 6).
| Characteristics | Controls n=258 | Cases N=86 | Total N=344 | ||||
|---|---|---|---|---|---|---|---|
| count | % | count | % | count | % | ||
| Labor Status | Spontaneous | 246 | -95.3 | 81 | -94.2 | 327 | -95.1 |
| Induced | 12 | -4.7 | 5 | -5.8 | 17 | -4.9 | |
| Mode of current delivery | Spontaneous vaginal delivery | 183 | -70.9 | 49 | -57 | 232 | -67.4 |
| Instrumental | 10 | -3.9 | 2 | -2.3 | 12 | -3.5 | |
| Caesarean section | 65 | -25.2 | 35 | -40.7 | 100 | -29.1 | |
| Complications during delivery? | no | 177 | -68.6 | 38 | -44.2 | 215 | -62.5 |
| yes | 81 | -31.4 | 48 | -55.8 | 129 | -37.5 | |
| Referred from other facility | no | 187 | -72.5 | 24 | -27.9 | 211 | -61.3 |
| yes | 71 | -27.5 | 62 | -72.1 | 133 | -38.7 | |
| Multiple birth during current pregnancy | no | 255 | -98.8 | 81 | -94.2 | 336 | -97.7 |
| yes | 3 | -1.2 | 5 | -5.8 | 8 | -2.3 | |
Table 6: Delivery characteristics of the cases and controls, at Jimma University specialized hospital, Jimma, Ethiopia, 2015.
Results from bivariate and multi-variable logistic regression analysis
Variables considered for multiple logistic regression were those with a p-value <0.2 at bivariate analysis and these included Gravida, residence, referral status, complications during previous pregnancy, abortion history, adverse pregnancy outcomes history, medical complications, illness during current pregnancy, ANC utilization, number of ANC, TT vaccine, medication received, anemia status, delivery mode, delivery complications, parthograph used, multiple pregnancy, obstetric emergencies.
Accordingly; mothers who are referred for delivery service from other area are more than five times to have adverse pregnancy outcomes than mothers who are not referred, AOR=5.49 95% CI [2.80-10.76]. Additionally, mothers who had illness during current pregnancy are seven times to be case than controls, AOR=7.22, 95% CI=1.65-31.58. Mothers who attend ANC were 83% less likely to have adverse pregnancy outcome, than mothers who didn’t attended ANC follow up, AOR = 0.17 95% CI [0.06-0.49]. Pregnant mothers who are anemic or had hemoglobin level of less than 11 gram/dl are more than seven times to have adverse pregnancy outcomes than non-anemic pregnant mothers, AOR=7.29 95% CI=[2.85-18.67]. Additionally, women who had obstetric emergencies during current pregnancy, complications during current delivery, and multiple pregnancy are more than 18 times AOR =18.40[6.12-55.37], 2 times AOR=2.65[1.38-5.11] and 7 times AOR=7.59[1.49-38.65] to have adverse pregnancy outcomes than their counterparts respectively.
Discussion
This study was aimed to assess determinants of adverse pregnancy outcomes in Jimma university specialized hospital, Jimma Town, Oromia regional state. The finding of this study indicated the impact of referral from other facility for delivery service, illness during current pregnancy, having ANC visit, anemia (hemoglobin level below 11 gm/dl), having delivery complications, multiple pregnancies and obstetric emergency during current pregnancy on pregnancy outcomes. There were differences among the cases and controls in relation to the above variables. In this study the mean age of the study subjects were 26.01 for cases and 25.34 for the controls.
In this study stillbirth takes majority of adverse pregnancy outcomes accounting 62.7% of cases and this is in line with similar study done in mekele where it accounts 61.2% of adverse birth outcomes [4]. This is probably because most of the mothers of the cases (72.1%) in this study are referred with serious obstetric complications to this hospital arrived late.
Multiple logistic regression output of this study showed that referral of mother with complication from other facility for delivery service is significantly associated with adverse pregnancy outcomes (Table 7). According to findings of this study, 96% of urban mothers are not referred while 88% of referred mothers are from rural residence. This is consistent with the study done in mekele public hospitals which indicates that mothers who lived in urban are 76% less likely to develop adverse birth out come as compared to those mothers who lived in rural area [4].
| Controls n=258(%) | Cases n=86(%) | COR 95 %(CI) | AOR 95 %(CI) | ||
|---|---|---|---|---|---|
| Gravidity | One | 134(51.9) | 32(37.2) | 1 | 1 |
| 02-Apr | 111(43.0) | 43(50.0) | 0.28(0.12-0.69)* | 0.92(0.255-3.32) | |
| ≥ five | 13(5.0) | 11(12.8) | 0.46(0.19-1.1) | 0.74(0.21-2.61) | |
| Mothers residence | Urban | 174(67.4) | 28(32.6) | 1 | 1 |
| Rural | 84(32.6) | 58(67.4) | 4.29(2.55-7.22)* | 0.48(0.12-1.88) | |
| Illnesses during current pregnancy | No | 254(98.4) | 74(86.0) | 1 | 1 |
| Yes | 4(1.6) | 12(14.0) | 10.29(3.23-32.88)* | 7.22(1.65-31.58)** | |
| Medical illness before pregnancy | No | 254(98.4) | 78(90.7) | 1 | 1 |
| Yes | 4(1.6) | 8(9.3) | 6.51(1.91-22.21)* | 2.55(0.45-14.36 | |
Table 7: Multiple logistic regression output for socio demographic factors associated with adverse pregnancy outcomes at Jimma University specialized hospital, Jimma, Ethiopia, 2015.
This might be due to distance naturally prevents mothers from doing so even if they are knowledgeable of the benefits of antenatal care services but deprives them the opportunity for early identification and management of pregnancy related problems and may further influence their choice of place of deliver and also lack some health services on time. Additionally, 35(72.9%) of cases who are referred for delivery had obstetric complications during labor delivery time so referring mother with obstetric complication lately will increase risk of developing APOs by delaying appropriate service (Table 8).
| Characteristics | Controls n=258(%) | Cases n=86(%) | COR 95 % (CI) | AOR 95 % (CI) | |
|---|---|---|---|---|---|
| Any history of abortion? | No | 243(94.2) | 72(83.7) | 1 | 1 |
| Yes | 15(5.8) | 14(16.3) | 3.15(1.45-6.83)* | 2.18(0.67-7.06) | |
| APOs history | No | 247(95.7) | 74(86.0) | 1 | 1 |
| Yes | 11(4.3) | 12(14.0) | 3.64(1.54-8.59)* | 1.85(0.45-7.59) | |
| ANC follow-up | No | 11(4.3) | 17(19.8) | 1 | 1 |
| Yes | 246(95.3) | 68(79.1) | 0.179(0.08-0.40)* | 0.17(0.06-0.49)** | |
| Received TT injection? | No | 12(4.7) | 21(24.4) | 1 | 1 |
| Yes | 154(59.7) | 43(50.0) | 0.93(0.87-0.99)* | 0.94(0.86-1.02) | |
| Medication taken during this pregnancy | No | 256(99.2) | 83(96.5) | 1 | 1 |
| Yes | 2(.8) | 3(3.5) | 4.63(0.76-28.16) | 0.45(0.04-5.4) | |
| Anemia status | non anemic | 249(96.5) | 59(68.6) | 1 | 1 |
| anemic | 9(3.5) | 27(31.4) | 12.66(5.66-28.35)* | 7.29(2.85-18.67)** | |
| Obstetric Emergency at current pregnancy | No | 252(97.7) | 67(77.9) | 1 | 1 |
| Yes | 6(2.3) | 19(22.1) | 11.9(4.58-31.0)* | 18.40(6.12-55.37)** | |
Table 8: Multiple logistic regression output for obstetric and gynecologic factors associated with adverse pregnancy outcomes at Jimma University specialized hospital, Jimma, Ethiopia, 2015.
Illness during current pregnancy was significantly associated with poor pregnancy outcomes [AOR 7.22 CI (1.65-31.58)]. This finding is consistent with similar study done in Kenya [5] and this may be medical illness present during pregnancy time affect maternal health as well as fetal growth and development.
Results of this study showed that, mothers who had ANC attendance were 83% less likely to have adverse pregnancy outcome, than mothers who didn’t attended ANC follow up, AOR = 0.17 95% CI [0.06-0.49]. During ANC follow up women will have access to information related to nutrition, danger signs of pregnancy, birth preparedness and complication readiness. Regular ANC follow up will also help a pregnant woman seek early treatment for her potential pregnancy related problems but if failed to showed up for ANC, she will be disadvantaged. This finding is in agreement with study done in Wollo [6] and Gondar university hospital [7] where mothers who didn’t attend ANC are more than 3 and 9 times at risk to develop adverse pregnancy outcomes respectively.
Anemia is significant predictor of adverse pregnancy outcome in this study where anemic mothers are more than 7 times at high risk to develop than those who are not anemic. This is similar with study done in Tanzania which indicates that low hemoglobin level is associated with the occurrence of low birth weight [8]. This might be low Hb levels during pregnancy leads to intra-uterine oxygen inadequacy and reduced iron stores, causing infantile anemia before the age of six months.
This study shows that those mothers who developed obstetric emergencies during pregnancy are more than 18 times at risk to develop adverse birth outcomes as compared to mothers who don’t develop obstetric emergencies during current pregnancy. This finding is in line with the study done in Kenya where mothers who develop obstetric emergencies are about 14 times at high risk of developing poor pregnancy outcomes compared to the controls [5-10]. This is because, obstetric emergencies like APH, pre eclampsia/eclampsia, cord prolapse, and fetal distress affect both maternal and fetal conditions and usually leads to occurrence of adverse pregnancy outcomes if they are not addressed timely.
The result also shows that mothers who develop complication during labor & delivery are 2.65 times more likely to develop adverse pregnancy outcome as compared to those mothers who don’t develop complication during labor and delivery AOR=2.65 CI (1.38-5.11).
According to the cross tabulation result 35(72.9%) of mothers who develop complication during labor and delivery among cases are referred from other facilities for delivery service. So those mothers who are referred with complications maybe delayed to get the right care on time leading to development of adverse pregnancy outcomes. This finding is consistent with similar study done in mekele public hospitals which shows that mothers who had complications during pregnancy and labor delivery are 4.85 and 9.94 times more likely to develop adverse birth outcomes than mothers who did not have complications during pregnancy and labor-delivery respectively [4]. This is also similar with study done in Gondar university hospital which showed that Obstetric emergencies such as postpartum hemorrhage (PPH), antepartum hemorrhage, cord prolapse and cord presentation, uterine rupture are significantly associated with poor pregnancy outcomes [7].
Multiple births affect the occurrence of adverse pregnancy outcomes by 7.59 folds compared to singleton pregnancies. This finding is supported by study done in Gondar university hospital which showed that, which showed that, mothers with multiple pregnancy are 2.26 times more at risk to give low birth weight baby and Stillbirth is significantly associated with preterm and low birth weight with AOR= 4.47 CI (1.39–14.32) and AOR = 18.21 CI (6.06 - 55.34) respectively [7]. This might be, multiple fetuses growing in the uterus will share the same supply form the mother and are at risk to be low birth weight. Additionally multiple pregnancy is usually leads to preterm birth which is also associated with development of stillbirth.
In Contrary to the above birth outcome predictors; gravidity, residence, complication during previous pregnancy, history of abortion, history of adverse pregnancy outcomes, pre-existing medical conditions, having tetanus injection, medication taken during current pregnancy, modes of delivery and parthograph use were significant predictors by the bivariate analysis which are not significant during the multiple logistic regression analysis (Table 9).
| Characteristics | Controls n=258(%) | Cases n=86(%) | COR(CI) | AOR(CI) | |
|---|---|---|---|---|---|
| Referred from | No | 187(72.5) | 24(27.9) | 1 | 1 |
| other facility for delivery service | Yes | 71(27.5) | 62(72.1) | 6.80(3.95-11.73)* | 5.49(2.80-10.76)** |
| Mode of current delivery | SVD | 183(70.9) | 49(57.0) | 1 | 1 |
| Instrumental | 10(3.9) | 2(2.3) | 0.497(0.30-0.84)* | 2.06(0.81-5.23) | |
| C/S | 65(25.2) | 35(40.7) | 0.37(0.08-1.79) | 0.40(0.04-3.60) | |
| Complications during delivery? | No | 177(68.6) | 38(44.2) | 1 | 1 |
| Yes | 81(31.4) | 48(55.8) | 2.76(1.67-4.55)* | 2.65(1.38-5.11)** | |
| Parthograph use | No | 244(94.6) | 85(98.8) | 1 | 1 |
| Yes | 14(5.4) | 1(1.2) | 0.21(0.03-1.58) | 0.15(0.01-1.73) | |
| Multiple birth | No | 255(98.8) | 81(94.2) | 1 | 1 |
| Yes | 3(1.2) | 5(5.8) | 5.25(1.23-22.44)* | 7.59(1.49-38.65)** | |
| Gender of the new born | Female | 100(38.8) | 42(48.8) | 1 | 1 |
| Male | 158(61.2) | 44(51.2) | 0.66(0.41-1.08)* | 0.61(0.31-1.20) | |
NB: * shows significant in bivariate logistic regression and ** indicates variables found to be predictor of the outcome variable in multiple logistic regression.
Table 9: Multiple logistic regression output for delivery related factors associated with adverse pregnancy outcomes at Jimma University specialized hospital, Jimma, Ethiopia, 2015.
This finding is different from findings of studies conducted on adverse pregnancy outcomes in other areas where these independent factors were identified to be predictors of adverse pregnancy outcomes (5, 7, 4 and 10). This deviation may be due to differences in study settings which includes, time, place and study design.
Limitation of the Study
• Unavailability of some independent variables on records which may have impact on the dependent variable (educational status, occupation, income, religion…).
• Exclusion of participants who do not have complete information could have resulted in selection bias and thus impacted on the results. Selection bias could have affected the accuracy of the data collected as the participants were sampled from hospitals.
Conclusion
In conclusion, this study has found that stillbirth was the highest among adverse pregnancy outcomes and On the other hand, low birth weight was the second most adverse birth outcome followed by preterm birth from births takes place in Jimma university hospital in 2015.
This study also indicates that; late referral of mother with complication, illness during current pregnancy, having ANC attendance, anemia during current pregnancy, complication during labor-delivery, multiple pregnancies and having obstetric emergencies were found to be statistically significant and these factors were possible predictors of adverse pregnancy outcomes. Having ANC attendance is determinant factor identified as preventive factor to adverse pregnancy outcomes.
On the other hand; gravidity, residence, complication during previous pregnancy, history of abortion, history of adverse pregnancy outcomes, pre-existing medical illnesses, having tetanus injection, medication taken during current pregnancy, modes of delivery and parthograph use were not found to be associated with adverse pregnancy outcomes.
Recommendations
• To Jimma zone health department; To monitor provision of quality focused ANC within the health facilities found in the zone and Monitor early referral in case of complications.
• For Jimma university specialized hospital; Creating good referral linkage with health facilities within its catchment areas including feedbacks provisions and Providing the most quality service for mothers coming for delivery service to decrease delay.
• To researchers; to do similar research using primary data supported with qualitative findings by addressing health facility related factors contributing to adverse pregnancy outcomes.
Acknowledgements
The authors would like to thank Jimma University College of health sciences for sponsoring this study and securing ethical clearance. Additional thanks will go to Jimma university specialized hospital and obstetric ward head for allowing the data collection procedures. My great gratitude finally goes to my advisors Mulumebet Abera and Amanuel Tesfay for their irreplaceable support throughout the whole work with their valuable advises.
Authors’ Contributions
Eyosiyas Yeshialem designed the study, participated in the data collection, performed analysis and interpretation of data. Mulumebet Abera and Amanuel Tesfay assisted in the design, approved the proposal with some revisions, participated in data analysis and revised subsequent drafts of the paper. Nigus Alemnew and Eyosiyas Yeshialem prepared the manuscript. All authors read and approved the final manuscript.
Conflict of Interest
Authors have declared that there are no conflicts of interest for this article.
References
- Vibal chaiba B (2014) Determinants of adverse pregnancy outcomes in Mutare district clinics. Inter J Obstetrics Gynaeco.
- World Health Organization (1984) the incidence of low birth weight: an update, Wkly Epidemiol Rec.
- Althabe F, Bhutta Z, Blencowe H, Chandra-Mouli V, Chou D, et al. (2012) In Born too soon: The global action report on preterm birth, Edited by Christopher Howson MK, Joy L. Geneva, Switzerland: WHO.
- Kent H, Johnson K, Curtis M, Hood JR, Atrash H (2006) Atlanta, GA: National center on birth defects & developmental disabilities. Proceedings of the Preconception Health and Health Care Clinical, Public Health, and Consumer Workgroup Meetings, Atlanta.
- Joyce Jebet C (2012) Poor pregnancy outcomes in public health facilities in Kenya, AFRICAN journal of midwifery and women’s health.
- Hailemariam B (2013) Factors associated with patterns of birth outcomes at public hospitals in mekele town, Ethiopia, Intern J Therap Applican 12: 39-46.
- A Eshete (2013) Birth outcomes among laboring mothers in selected health facilities of North Wollo Zone A. Eshete et al. Health 5: 1141-1150.
- Adane A (2014) Adverse birth outcomes among deliveries in Gondar university hospital 14: 90.
- Nybo Andersen AM, Wohlfahrt J, Christens P, Olsen J, Melbye M (2000) Maternal age and fetal loss: population based register linkage study. BMJ 320: 1708-1712.
- Ziyo FY, Matly FA, Mehemd GM, Dofany EM (2009) Relation between Prenatal care and Pregnancy Outcome at Benghazi, Sudanese. J Publi Health 4: 4.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences