Hernia de Bochdalek: A Challenging Diagnosis
Campos-Sanchez Eduardo Jose, Mejia-Martinez Lessdy Aarely, Sierra-Aguilar S Ivana, Avila-De La Puente Claudia and Juan Francisco Ayestas
DOI10.21767/2471-299X.1000072
1Doctor of Medicine and Surgery, Faculty of Medical Sciences, National Autonomous University of Honduras, Honduras
2Specialist Doctor in General Surgery, Laparoscopy and Wall Surgery Abdominal, Honduras
- *Corresponding Author:
- Mejia-Martinez LA
Doctor of Medicine and Surgery
Faculty of Medical Sciences
National Autonomous University of Honduras
Honduras
Tel: +50432829844
E-mail: less_aarely@hotmail.es
Received Date: July 22, 2018; Accepted Date: September 06, 2018; Published Date: September 13, 2018
Citation: Campos-Sanchez EJ, Mejia-Martinez LA, Sierra-Aguilar SI, Avila-De LPC, Juan FA (2018) Hernia de Bochdalek: A Challenging Diagnosis. Med Clin Rev 4:10. doi: 10.21767/2471-299X.1000072
Copyright: © 2018 Campos-Sanchez EJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Diaphragmatic hernias are defined as a transposition of abdominal organs into the thoracic cavity through a defect in the phrenic muscle. They can be classified as congenital, acquired, or post traumatic. The Bochdalek hernia is congenital, it is produced by an alteration in the embryological development of the diaphragm, causing a zone of anatomical weakness that allows the protrusion of intraabdominal organs into the thoracic cavity. The prevalence of the Bochdalek hernia is 1 in 2,200 births and is located on the left side 80%-90% of the time, only 5%-10% remain undetectable during childhood. Less than 100 cases have been reported in adults. In Honduras there have been few cases reported in pediatrics, and none in adults. We present the case of a 38-year-old patient that seeks at the Hospital Escuela Universitario in Tegucigalpa, Honduras, due to abdominal pain located in the left iliac fosse that irradiates to the right flank and hypochondrium over the past two months, accompanied by dyspnea and paroxistic episodes of cough. At thoracic auscultation wheezing was found with predominance in the left lung, with hypoventilation and the presence of intestinal sounds. A thoracoabdominal tomography with contrast was performed, finding the presence of a diaphragmatic hernia occupying the whole left hemithorax, including the spleen, colon and stomach. The data is corroborated by a diagnostic laparoscopy, but because the organs could not be reduced to the abdominal cavity a laparotomy was performed. The findings correspond to the organs that are commonly herniated in the left Bochdalek hernia. After the laparotomy the patient had a satisfying progress, with subsequent hospital discharge. It is important to have a timely diagnosis and adequate treatment for this type of hernia to prevent complications that could compromise the life of the patient.
Keywords
Diaphragmatic hernia; Bochdalek; Adult
Introduction
The first appointment of a diaphragmatic hernia was made by Ambrosio Paré in 1579, and originally described by Lazarus Riverius in 1679, who described his pos-mortem finding in a 24-year-old man. Charles Holt was the first to describe it in the child, and Vincent Alexander Bochdalek, in 1848, described from the embryological point of view the herniation of the intestine by a diaphragmatic dorsal foramen, a variety that today bears his name [1]. In the review of the world literature we find 130 reported cases of Bochdalek hernia in the adult [2]. In Honduras there are few reported cases in pediatrics and no case reported in adults according to the database of publications made to date. The incidence is approximately 1 in every 2,200-12,500 live births. Bochdalek hernia is rare in adults and represents 0.17%-6% of all diaphragmatic hernias [3,4].
Diaphragmatic hernias can be defined as the transposition of abdominal organs to the thoracic cage, through defects of the phrenic muscle. They can be classified as congenital (such as those of Morgagni-Larrey, Bochdalek), acquired (such as different types of hiatal hernia) or post-traumatic (due to a closed contusion or a lacerating lesion) [5]. Bochdalek hernia from the anatomopathological point of view is produced by an alteration in the embryological development of the diaphragm between week 8 and 10 of gestation characterized by a defect in the closure of the pleuroperitoneal duct preventing a complete fusion of the elements lumbar (posterior) and costal (lateral). The resulting consequence is a weak anatomical zone that allows the protrusion of the intra-abdominal organs towards the thoracic cage through the diaphragm [6]. They are located 80%-90% on the left side and the defect is usually about 2 cm, located just above the adrenal gland [7]. The content of the Bochdalek hernia varies depending on the affected side: on the right, the liver, right kidney and fat are involved; however, when the defect is left, it may contain the digestive tract, spleen, liver, left kidney, pancreas or omentum [1].
When this pathology is not detected in the neonatal stage, the patient adapts chronically to this condition and can reach adulthood completely asymptomatic. When the symptoms appear, they are usually progressively predominating those of non-specific digestive type such as nausea, early postprandial fullness, bleeding from the digestive tract, epigastric pain, melena and others such as respiratory difficulty after food intake and weight loss [6]. The patient may report significant chest pain due to an early complication, such as respiratory compromise due to atelectasis or pneumonia, or late complications such as volvulus, with possible rupture of an abdominal viscus within the thorax [4].
The diagnosis of Bochdalek hernia in the adult can be established in two ways: a) by incidental finding in chest X-ray studies, or b) by the presence of complications secondary to the passage of abdominal viscera through the diaphragmatic orifice, which can produce incarceration, strangulation and/or rupture of these within the thorax [2]. The treatment of diaphragmatic hernias is surgical. The approach can be done by laparotomy, thoracotomy or combined, depending on the presence or absence of complications [7]. The repair of the hernia can be done by transthoracic or abdominal route, currently it can be with minimal invasion or in a conventional way. The transabdominal route gives the surgeon the advantage of confirming the position of the abdominal viscera and their commitment; the procedure of choice will depend on the surgeon and his experience. Reduction of the viscera to the abdominal cavity and closure of the diaphragmatic gap prior to the installation of a pleural drainage [8].
Clinical Case
38-year-old female patient, housewife, from Tegucigalpa, Honduras who came to the emergency of Surgery University Hospital University located in that city. Patient with a history of alcoholism and smoking of 12 years of evolution, presented abdominal pain of 2 months of evolution in the left iliac fossa radiating to the flank and right hypochondrium, of progressive insidious onset, of mild to moderate intensity, sometimes it did not yield with analgesics, accompanied by dyspnea of small to medium efforts and paroxysmal episodes of cough, without cyanosis.
Physical examination revealed: lucid, conscious patient, Glasgow 15/15, blood pressure 110/70 mmhg, heart rate 78 per minute, respiratory rate 20 per minute, oxygen saturation 96%, weight 61.8 kilograms, height 1.55 meters, index of body mass 25.7 kg/m3, at thoracic auscultation was found: Wheezing predominance in the left lung field, hypoventilation of the left base and bowel sounds in the left lung.
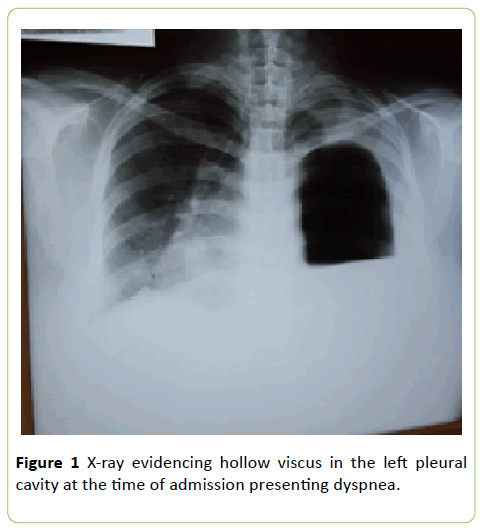
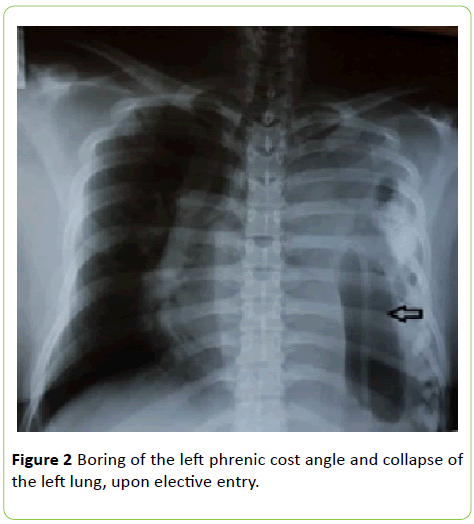
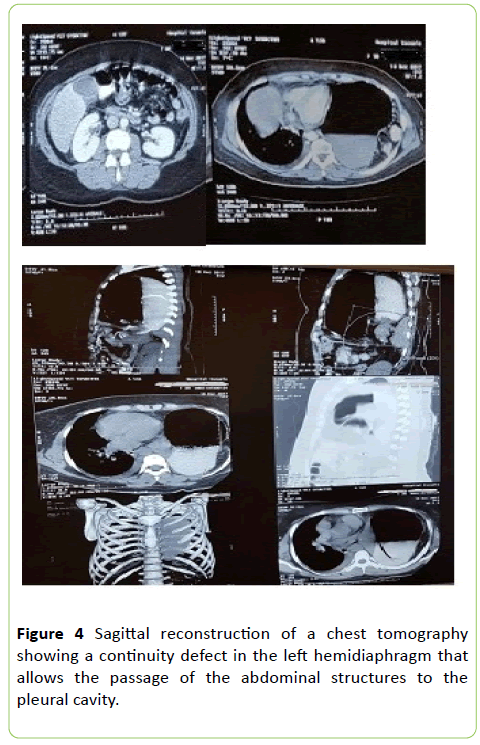
At the time of admission, the patient presented with a dyspnea and on X-rays the presence of a hollow viscus was evident in the left pleural cavity (Figure 1), for which a thoracic drainage tube was placed. Spirometry reported: FVC (L): 0.86, FEV 1 (L): 0.80, FEV1/FVC: 93%, FEF 25%-75% (L/sec): 1.00 although FEV1 and FEF 25%-75% are reduced, the FEV1/FVC ratio is high, in conclusion, a severe obstructive pathology of the respiratory tract was diagnosed. Ultrasound revealed free fluid in the right iliac fossa with a volume of 13 cc. The patient who until now was in the internal medicine service is transferred to the general surgery service, where a new X-ray was performed, which reported effacement of the left phrenic cost angle and collapse of the left lung (Figure 2). Subsequently, in the thoracoabdominal tomography with contrast medium, a diaphragmatic hernia was found occupying the entire left hemithorax, observing the colon towards the apical portion, stomach and spleen in the region of the thorax, as well as the tail of the pancreas. There are mediastinal structures displaced to the right, right main bronchus decreased in caliber, without evidence of segmental bronchi, showing total left lung collapse. A left pleural effusion was also observed with basal laminar atelectasis, scarce free fluid in the left and right slider, being more accentuated towards the pelvic cavity. The gastric chamber was dilated and localized in the left hemithorax (Figure 3).
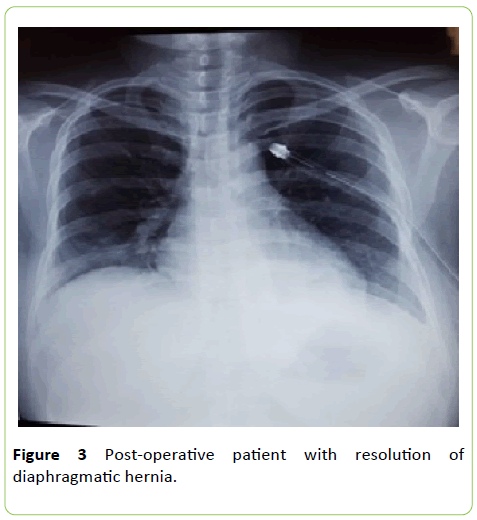
The endoscopic findings were: esophagus (lumen and mucosa) normal, gastroesophageal junction and Z line in 37 centimeters, motility and normal lower esophageal sphincter, stomach (fundus, body, angle, antrum and pylorus) normal; Duodenum, bulb and second normal portion. The blood gases reported: PCO2 29 mmhg and PO2 63 mmhg both decreased, PH 7.44, HCO3 19.6 mml/L, in the blood count the white blood cells were found in 18.6 × 103/μl. It was diagnosed as a grade IV left diaphragmatic hernia; the patient was treated in the ward, compensating the ventilatory part, and later scheduled her surgery, tentatively by laparoscopy. She was discharged in a better general condition, tolerating environmental oxygen and diet, and was scheduled to meet in 2 weeks to schedule her surgery selectively. Diagnostic laparoscopy was programmed to reduce structures to the abdominal cavity and repair the diaphragmatic defect. During the surgery there was an inability to reduce the structures to the abdominal cavity, so it was decided to convert the procedure to an open one, with an incision in the supra umbilical midline. The transoperative findings were: Diaphragmatic defect in the left posterior region of about 6 centimeters in length, stomach, spleen, splenic flexure of the colon and omentum in the left pleural cavity with multiple adhesions, without contamination of the pleural cavity, left lung collapsed, what was placed chest tube on the left side, 28 French. In the postoperative period, the patient presented with hypoxemia and decreased arterial blood gases, so she was left under observation for 24 hours with the following medical orders: Quantification of nasogastric tube production, chest tube, oxygen mask with reservoir at 10 liters per minute, ampicillin/sulbactam 1.5 grams intravenously every 8 hours, amikacin 500 mg intravenously every 12 hours, enoxaparin 40 milligrams subcutaneously at 6 hours postoperatively in single dose, metoclopramide 10 milligrams for necessary reasons, saline 0.9% 1000 ml plus dexketoprofen 150 milligram ampoule in serum every 8 hours, the 0.9% saline solution is changed to Hartman solution or Ringer's lactate due to changes in PH. After the observation period, she moved to women's surgery room B. On the third post-operative day, since hypoventilation areas were not clinically observed and the vesicular murmur was present in both pulmonary fields, it was decided to remove the thoracic tube. On the fifth hospital day in view of the good clinical evolution, tolerating the oral route, environmental oxygen and chest X-rays, observing that there was no pleural effusion and presence of good lung expansion, without an area of pneumothorax or atelectasis (Figure 4), it was decided to leave the health center.
Discussion
The prevalence of Bochdalek hernia is 1 in 2,200 births and only 5%-10% of them remain undetectable in childhood [9]. Less than 100 cases have been reported among adults. The symptoms in adults are chronic and varied [10]. Circumstances that may favor the delay of the manifestation of symptoms would be the ease of mobility of the abdominal viscera towards the thoracic cavity. Symptoms are generally nonspecific, with respiratory and digestive manifestations being the most frequently described [11]. The hernia of Bochdalek is a rare hernia in adults, therefore, its misdiagnosis is common. Inappropriate interventions, such as the placement of a chest tube, can occur in cases of misdiagnosis. The delay in diagnosis can conclude in strangulation and death [9]. In this case, according to the literature, the patient goes to the emergency room with abdominal pain, cough and dyspnea; symptoms that had presented 2 months in advance and whose diagnosis in the first instance was of obstructive pathology of the severe respiratory tract.
Computed tomography is the most accurate of the imaging modalities for the diagnosis and evaluation of hernia contents, especially when it is small. The other advantage of computed tomography is that it can detect the presence of the spleen as one of the contents and help in the cautious management of this friable organ to prevent a catastrophe [9]. The diagnosis of the patient in this case was made by means of computed tomography, where the presence of the spleen, colon and stomach in the left hemithorax was observed, data that later were corroborated when performing the surgical procedure and which agrees as Common findings of organs that herniate in left Bochdalek hernias as discussed in the introduction, according to the literature. Bochdalek hernia is more common on the left side (80%-85%), because complete closure occurs on the right side before on the left side and the liver usually obstructs against right side herniation [12]. In approximately 10%-38% of cases, a sac is present, which can rupture in adult life with the appearance of acute symptoms of strangulation [13].
The management of the Bochdalek hernia consists in the surgical reduction of the herniation in the abdominal cavity and in the repair of the diaphragmatic defect as soon as possible. Traditionally, it can be performed by laparotomy or thoracotomy, this depends on the scenario. Recently, in order to minimize surgical trauma, thoracoscopic or laparoscopic repair of the Bochdalek hernia has also been reported, with excellent results [14]. Laparoscopic technique has gained popularity, especially in elective cases [15]. In this case, the patient was electively scheduled for laparoscopy, which could not be performed due to the inability to reduce the structures to the abdominal cavity, which ended in laparotomy.
The early diagnosis is of vital importance to avoid possible complications that endanger the life of the patient and thus be able to initiate an opportune handling with the appropriate intervention.
Conflict of Interest
The authors declare no conflict of interest with the publication of this article.
References
- Ferrero Moreira ME, Martinez Ortega E, Valle Garrido L, Gonzales YE, Cárdenas HMM (2013) Intestinal occlusion by Bochdalek hernia, Revista Cubana de Pediatría 85: 529-538.
- Cabrera Santos J, Hidalgo Maldonado M, Segovia EB, Quezada C (2014) Bochdalek diaphragmatic hernia in the adult: Case report. J Faculty Med Sci Univer Cuenca 31: 76-81.
- Tavares FLS, AsCBC-ES, Tavares MB, Pimentel MC (2016) Congenital diaphragmatic hernia in adults. Revista do Colegio Brasileiro de Cirurgiὁes 4: 1-3.
- Souza LEA, Anjos KLS, Sousa DO, Loureiro GJF, Centeno DM, et al. (2018) Symptomatic Bochdalek hernia in adult: A case report. Inter Arch Med 11: 1-3.
- King DR (2015) Hernia of Bochdalek. American J Resp Med 2: 137-138.
- Castro-Pérez J, Quintero-Tlapalamatl J, Morales-Domínguez A, Urbina-Ramírez A (2016) Elective surgery of Bochdalek hernia in an adult woman, case report. J Res Develop Heal Tlax 2: 16-19.
- Parra M, Ortega SM, Berríos SR, de Ossó AJT (2013) Diaphragmatic hernia complicated with hollow viscera rupture within the thoracic cavity. Revista Chilena de Cirugia 65: 342-345.
- Cruz Cantu LM, Lezama de Luna JF, Samano Robles CM (2016) Bochdalek hernia complicated with gastric perforation in an adult patient. Report of a case. Surg Gen Magaz 38: 88-91.
- Saroj SK, Kumar S, Afaque Y, Bhartia AK, Bhartia VK (2016) Laparoscopic repair of congenital diaphragmatic. Minim Invas Surg 2: 1-5.
- Herling A, Makhdom F, Al-Shehri A, Mulder D (2014) Bochdalek hernia in a symptomatic adult. Ann Thora Surg 98: 701-704.
- Flores S, Alba R, Galindo F, Reyes M (2016) Congenital diaphragmatic hernia of late presentation. Frequency and experience in the possibilities of surgical medical treatment. Mater Child Res Arch Mag 8: 48-54.
- Kikuchi S, Nishizaki M, Kuroda S, Kagawa S, Fujiwara T (2016) A case of right-sided Bochdalek hernia incidentally diagnosed in a gastric cancer patient. BMC Surgery 16: 34.
- Banchini F, Santoni R, Banchini A, Bodini FC, Patrizio Capelli (2016) Right posterior diaphragmatic hernia (Bochdalek) with liver involvement and alteration of hepatic outflow in adult: a case report. Springerplus 5: 1561.
- Cindolo L, Berardinelli F, Manzi A, Spagnuolo F, Fabbri E, et al. (2015) Intraoperative presentation of Bochdalek's hernia in an adult during robotic-assisted partial nephrectomy: An uncommon situation and literature review. Archivio Italiano di Urologia e Andrologia 87: 327-329.
- Harada M, Tsujimoto H, Nagata K, Ito N, Yamazaki K, et al. (2016) Successful laparoscopic repair of an incarcerated bochdalek hernia associated with increased intra-abdominal pressure during use of blow gun: A case report. Int J Surg Case Rep 23: 131-133.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences