Laparoscopic Myomectomy: A 6-Year Experience at Nordica Fertility Center, Lagos, Nigeria
Abayomi Ajayi, Victor Ajayi, Oluwafunmilola Biobaku, Ifeoluwa Oyetunji, Happiness Aikhuele, Oladapo Adejuwon and Bamgboye M Afolabi
DOI10.21767/2471-299X.1000015
1Nordica Fertility Center, 106 Norman Williams Street, Ikoyi, Lagos, Nigeria
2Health, Environment and Development Foundation, 34 Montgomery Road, Yaba, Lagos, Nigeria
- *Corresponding Author:
- Bamgboye M Afolabi
Health, Environment and Development Foundation 34 Montgomery Road,Yaba, Lagos, Nigeria
Tel: +234(0) 803 049 0729, +234803 600 3300
E-mail: bmafolabi@gmail.com, yomi.ajayi@nordicalagos.org
Received Date: Dec 04, 2015; Accepted Date: Feb 10, 2015; Published Date: Feb 15, 2015
Citation: Victor A,Oluwafunmilola B, Ifeoluwa O,Laparoscopic Myomectomy: A 6-Year Experience at Nordica Fertility Center,Lagos, Nigeria.Med Clin Rev. 2015, 2:6. doi: 10.21767/2471-299X.1000015
Copyright: © 2016 Ajayi A,et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Abstract
Setting: Nordica Fertility Center, Lagos, Nigeria.
Patients: Thirty-one consecutive Infertile Women (IW) with myomas.
Intervention: Laparoscopic myomectomy.
Main outcome measures: Pattern of myomas, complications, live births.
Results: In all, 139 histologically confirmed myomas were removed from 31 IW (means (±) of age = 38.03 [5.3] and of Body Mass Index = 27.38 [4.6]) during laparoscopic myomectomy (LM) for symptomatic uterine myoma. Infertility was primary and secondary in 13 (41.9%) and in 18 (58.1%) cases respectively and their mean duration of trying to conceive was 5.69 (3.5) years. Six (19.4%) of these women had undergone previous abdominal uterine surgery including LM (2, 6.4%), open myomectomies (3, 9.7%) and appendectomy (1, 3.2%). The range of uterine size was 10-24 weeks. Fibroids were observed more in multiple sites (15, 48.4%) than intramural (10, 32.3%) or sub-serous (4, 12.9%) alone. Two (6.4%) fibroids were exclusively pedunculated. The largest number of fibroid seedlings removed from a patient was 14 and median diameter of the fibroids was 7 cm. Seven (23.0%) patients had post- operative complications two amongst whom had hemorrhagic complications including one hematoma and one excessive hemorrhage warranting conversion to open laparotomy in 1 (3.2%) patient. There was no association between previous abdominal surgeries, body mass index and the rate of complications. Overall mean blood loss was 399 mls (± 338 mls). Three (9.7%) women required post operation blood transfusion. Mean length of hospital stay was 2.77(± 1.43) days. After hysteroscopy at 8 weeks post LM, 14 (45.2%) of these women proceeded to in-vitro fertilization (IVF) treatment and 3 (21.4%) became pregnant and delivered live births, one with twins.
Conclusion: There is relatively low complication rate and short mean duration of hospital stay with LM. Recommendation: Considering the benefits of LM, it is recommended even in low resource settings like ours.
Keywords
Infertility; Fibroid; Laparoscopy; Pregnancy outcome; Lagos; Nigeria
Abbreviations
IVF: In Vitro Fertilization; IW: Infertile Women; LM: Laparoscopic Myomectomy; NFC: Nordica Fertility Center; TTC: Years of Trying to Conceive; GnRH: Gonadotropin-Releasing Hormone
Introduction
For many centuries past, fibroids (myomas) have been very common tumors affecting women though; apparently no significant data exists to ascertain the cause or predisposing factor of myoma. Early authors regard myomas as the most common uterine neoplasm with a prevalence of approximately 20-25% in women in child-bearing age group [1]. Later study pointed out that myomas develop out of benign transformation and proliferation of smooth muscle cells of Müllerian origin such as the fallopian tubes, uterine corpus, and cervix [2]. Although these authors suggested that elevated estrogen stimulation alone or in concert with growth hormone or human placental lactogen possibly contribute as major growth regulators, other workers were of the view that progesterone appears to inhibit the growth of myomas but under certain conditions may promote their growth [3]. Questions have been asked whether fibroids have any impact on fertility and / or completion of gestation [4]. In search of an answer to this question, it is argued that diet, weight, hypertension and habits are risk factors that have bearing on fibroid and that fibroids produce prolactin, which, in presence of very high level of aromatase, provoke higher level of estradiol compared to women with normal myometrium [4]. This finding, they concluded, was detrimental to fertility. There has been little or no argument contrary to the fact that fibroid negatively impacts fertility. Studies have shown that fibroids occur in roughly 5-10% of the patients who are infertile, though fibroids are found to be the single identified factor in only 1-2.4% of the infertile patients. [5-9]. Several hypotheses have been put forward to explain the mechanisms by which fibroids can lead to infertility. Fibroids can cause distortion and enlargement of the endometrial cavity by submucous and intramural leiomyomas, with an intra-cavitary component affect implantation [10,11]. Implantation failure may also be explained by focal endometrial vascular disturbances, endometrial inflammation, and secretion of vasoactive substances [12,13]. Leiomyomas may also cause dysfunctional uterine contractility and interfere with sperm and ovum transport [12,14,15]. There is the possibility that intramural leiomyomas could also obstruct either or both tubal ostia. Alteration of the uterine cavity by either submucosal or deeply penetrating intramural fibroids is most prognostic of compromised fertility warranting consideration of myomectomy in the sub-fertile patient [16]. The procedure of laparoscopic myomectomy was first described in 1979, specifically for subserous fibroids but as from the early ‘80s till date, it has been one of the everyday surgical procedures [17]. Though a school of thought stipulates that the maximal size of fibroid must be 8-10 cm and the total number of fibroids should not exceed four [18], there is yet no definitive criteria on the size and number of myomas to be removed by laparoscopic myomectomy. While some authors suggest a single intramural or subserosal fibroid ≤ 15 cm in size or a maximum of three fibroids of ≤ 5 cm [18], others believe in an individual choice based on pathological findings and surgical skill [19]. Location of the fibroid may be a major determinant in infertility and may also be a concern to the surgeon. Intramural and subserosal fibroid that are large enough may distort the uterine cavity and eventually interfere with the product of conception achieved either naturally or through assisted reproduction cycles [20]. An earlier work however claims that fibroids that are pedunculated may have little or no detrimental effects on fertility [21]. Being an invasive procedure, laparoscopic myomectomy has its own risks depending on the number (> 3 fibroids), location (intra-mural or intra-ligamentous) and size of the myomas with size being the particular factor that influence risk of major complications [22]. Uterine rupture during pregnancy and / or labor, observed at a prevalence of 5.3%, has been reported as a major risk factor of myomectomy at laparoscopy or laparotomy [23], though a study recommended caesarian section should more than 50% of the myometrium be disrupted during any of these procedures [24]. Both intra- and post-operative complications associated with laparoscopic myomectomy have been documented [25] which include bladder, bowel, and ureteral injury, hemorrhage requiring transfusion, and unintended conversion to hysterectomy, fistula, thrombosis, and embolism. Interestingly, a randomized control trial reported that laparoscopic myomectomy significantly lessened, among others, mean decline in hemoglobin, time to hospital discharge and the percentage of women requesting analgesics, as compared to minilaparotomy 26]. What gynecologists wished is the management of fibroids such that it would no longer be a burden to women who wish to still become pregnant or to the health of women in general. Laparoscopic myomectomy has been considered to be a safe technique with an extremely low failure rate and good results in terms of outcome of pregnancy [27]. This procedure is also beneficial for patients with unexplained infertility since it is able to detect the cause(s) of infertility in the pelvic cavity and to design a suitable management plan for possible postoperative pregnancy [28]. There are few studies in Nigeria that document the number, sizes and location of fibroids presented by infertile women. Fewer still document the procedure of laparoscopic myomectomy for the excision of the fibroids and the complications of the procedure. The main objectives of the study were to describe the profile of women who had laparoscopic myomectomy, the characteristics of the fibroids removed, the complication rates, duration of hospital stay and pregnancy outcome in those that pursued infertility treatment after laparoscopic myomectomy.
Presented in this paper is a review of laparoscopic myomectomies conducted at Nordica Fertility Center (NFC) in Lagos, Nigeria.
Materials and Methodology
Setting
A retrospective and observational study in which a detailed review of records of 31 consecutive infertile women who had laparoscopic myomectomy was conducted between 2008 and 2014. The setting was Nordica fertility center, Lagos Nigeria a leading assisted conception and endoscopy center. The study reviewed laparoscopic myomectomy in all 31 patients and fertility outcome in 14 of them who underwent in vitro Fertilization afterwards.
Data analysis
All statistical analyses were performed in Stata 13 (StataCorp, Texas 77845 USA). Chi-square test and Student’s ttest were used to analyze different variables. A P value of less than 0.05 was considered statistically significant.
The pre-operative work up included a detailed history and examination, blood work and a vaginal ultrasound. Eight weeks post laparoscopic myomectomy the women proceeding to IVF had hysteroscopy. All procedures were performed under general anesthesia.
Equipment
Standard laparoscopic equipment was used in a laparoscopic theatre in the endoscopy arm of Nordica Fertility Centre, Lagos. Images were displayed on a high definition screen and a 3D-chip camera was used. Hysteroscopy was performed using a rigid 30° 5-mm hysteroscope.
Procedure
Laparoscopy with multiple –port access was the main method performed. The area of the fibroid was infiltrated with vasopressin using 20IU in 30 ml normal saline solution to minimize blood loss. Monopolar cautery was used for the incision. After the myomectomy the bed was closed in single or multiple layers or by diathermy. The fibroids were retrieved by morcellation
Surgeons’ experience
Two experienced laparoscopic surgeons performed the procedures. Gynecological endoscopy was their main practice. Inclusion criteria were patients with subserous and / or intramural fibroids only and patients with fibroids less than 26 weeks. Exclusion criteria were patients with pregnancy coexisting with fibroid, fibroids bigger than or equal to 26 weeks and patients with severe anaemia.
Ethics approval
The study was approved by the State Ethics Committee on Health Research
Patients consent
Where appropriate and feasible, each participant in the study was contacted and all gave verbal approval for their data to be used in the research. In return, participants were assured of the confidentiality of their data and that the research will not use names of the subjects and that after three years, the data will be destroyed.
Results
Demographic characteristics
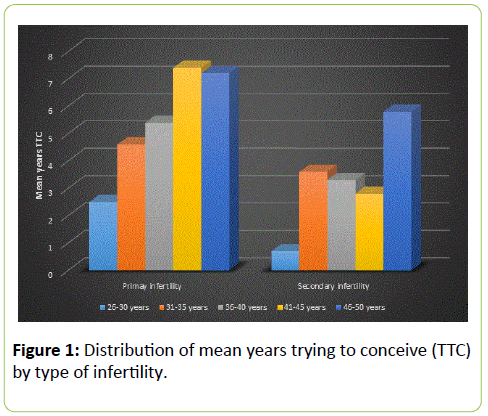
A total 139 histologically confirmed myomas, larger than 3 cm, were enucleated from 31 infertile women (means (± sd) of age and BMI of 38.0 (5.3) and 27.4 (4.6) respectively) most of whom were currently married (93.5%). These infertile women underwent laparoscopic myomectomies for symptomatic uterine myoma (Table 1). Infertility was primary in 13 cases (41.9%) and secondary in the remainder 18 cases (58.06%). The overall mean (± sd) years of trying to conceive (TTC) was 5.7 (3.5) which was significantly (t = -1.89, df = 22.1, p = 0.03) shorter in primary (4.3 ± 3.8) than in secondary (6.7 ± 3.0) infertility and in normal weight (4.3 ± 3.8) than in obese (7.4 ± 3.5) women. The longest years TTC was observed among those 41-45years old (7.4) and among obese women (7.4). Previous abdominal or uterine surgery was documented only among infertile women with secondary infertility among whom 3 (16.7%) had were open myomectomy, 2 (11.1%) had laparoscopic myomectomy and 1 (5.5%) had appendectomy. Occupational differentiations are as shown in the Table 1.
| All | Type of infertility | |||||
|---|---|---|---|---|---|---|
| (n = 31) | Primary (n = 13) |
Secondary (n = 18) |
t | df | p-value | |
| Mean (± SD) Age (years) | 38.0(5.3) | 37.4(5.3) | 38.5(5.4) | -0.56 | 26.3 | 0.28 |
| Mean (± SD) BMI (Kg/m2) | 27.4(4.6) | 26.1(5.0) | 28.3(4.1) | -1.3 | 22.7 | 0.1 |
| Mean(± SD) years TTCfor All | 5.7(3.5) | 4.3(3.8) | 6.7(3.0) | -1.89 | 22.1 | 0.03 |
| Mean(± SD) years TTCby age group | ||||||
| 26-30 | 2.5(0.7) | 2.0(0.0) | 3.0(0.0) | - | - | - |
| 31-35 | 4.6(3.6) | 1.5(1.3) | 6.4(3.2) | -5.86 | 23.9 | 0 |
| 36-40 | 5.4(3.3) | 5.4(3.5) | 5.5(3.5) | -0.08 | 26 | 0.47 |
| 41-45 | 7.4(2.8) | 0.0(0.0) | 7.4(2.8) | - | - | - |
| 46-50 | 7.2(5.8) | 5.8(7.4) | 10.0(0.0) | -2.05 | 12 | 0.03 |
| Mean(±SD) years TTCby BMI | ||||||
| Normal weight | 4.3(3.8) | 3.8(3.9) | 5.3(4.0) | -1.05 | 26.4 | 0.15 |
| Overweight | 5.6(3.2) | 3.0(2.1) | 6.7(2.9) | -4.12 | 29 | 0.0001 |
| Obese | 7.4(3.5) | 7.0(5.2) | 7.6(2.9) | -0.38 | 17.4 | 0.36 |
| Mean(± SD) years TTCby Marital status | ||||||
| Single | 1.0(1.4) | 1(1.4) | 0(0.0) | - | - | - |
| Married | 6.0(3.4) | 4.9(3.8) | 6.7(3.0) | -1.42 | 22.08 | 0.08 |
| Freq.(%) of Previous abdominal/uterine surgery | ||||||
| Appendectomy | 1(100.0) | 0(0.0) | 1(5.5) | - | - | - |
| Laparoscopic myomectomy | 2(6.4) | 0(0.0) | 2(11.1) | - | - | - |
| Open myomectomy | 3(9.7) | 0(0.0) | 3(16.7) | - | - | - |
| None | 25(80.6) | 13(100.0) | 12(66.7) | - | - | - |
| Freq.(%) of Occupation | ||||||
| Professional | 12(38.7) | 6(50.0) | 6(50.0) | - | - | - |
| Support service | 7(22.6) | 4(57.1) | 3(42.9) | - | - | - |
| Sales worker | 8(25.8) | 2(25.0) | 6(75.0) | - | - | - |
| Housewife | 1(3.2) | 0(0.0) | 1(100.0) | - | - | - |
| Student | 1(3.2) | 0(0.0) | 1(100.0) | - | - | - |
| Unemployed | 2(6.4) | 1(50.0) | 1(50.0) | - | - | - |
Table 1: Socio-demographic characteristics of women presenting for laparoscopic myomectomy according to type of infertility. TTC = Trying to Conceive.
Figure 1 is a graphical illustration of the age-dependent distribution of mean years TTC as observed in primary and in secondary infertility indication lack of consistence in this variable in the latter group.
Table 2 describes all the infertile women by their parity and number of miscarriages experienced relevant to their age group and Body Mass Index. Only those aged 41 years and above were parous, indicating secondary infertility amongst them. Of the 8 (25.8%) infertile women aged 41-45 years who presented for LM, 4 (50.0%) were nulliparous and 2 (25.0%) had parity of 1 and another 2 (25.0%) a parity of 4. Only 1 (33.0%) out of 3 women aged 46-50 years was parous, as shown in the table.
| Age group (years) | Body Mass Index | |||||||
|---|---|---|---|---|---|---|---|---|
| 25-30 | 31-35 | 36-40 | 41-45 | 46-50 | 18.5-24.99 | 25.0-29.99 | ≥30 | |
| Total (%) | 2(6.4) | 8(25.8) | 10(32.30) | 8(25.8) | 3(9.7) | 9(29.0) | 14(45.2) | 8(25.8) |
| Parity | ||||||||
| 0 | 2(100.0) | 8(100.0) | 10(100.0) | 4(50.0) | 2 (66.7) | 9(100.0) | 10(72.0) | 7(88.0) |
| 1 | 0(0.0) | 0(0.0) | 0(0.0) | 2(25.0) | 1(33.3) | 0(0.0) | 2(14.0) | 1(12.0) |
| 4 | 0(0.0) | 0(0.0) | 0(0.0) | 2(25.0) | 0(0.0) | 0(0.0) | 2(14.0) | 0(0.0) |
| No. of miscarriages | ||||||||
| 0 | 1(50.0) | 3(38.0) | 7(70.0) | 1(12.0) | 2(66.7) | 6(67.0) | 5(36.0) | 3(38.0) |
| 1 | 0(0.0) | 4(50.0) | 1(10.0) | 3(38.0) | 0(0) | 2(22.0) | 5(36.0) | 1(12.0) |
| 2 | 1(50.0) | 0(0.0) | 1(10.0) | 3(38.0) | 0(0.0) | 1(11.0) | 2(14.0) | 2(25.0) |
| 3 | 0(0.0) | 1(12.0) | 0(0.0) | 1(12.0) | 0(0.0) | 0(0.0) | 2(14.0) | 0(0.0) |
| 5 | 0(0.0) | 0(0.0) | 1(10.0) | 0(0.0) | 1(33.3) | 0(0.0) | 0(0.0) | 2(25.0) |
| Ratio | 1:1 | 0.9:1 | 0.8:1 | 1.5:1 | 1.7:1 | 0.4:1 | 1.1:1 | 1.9:1 |
Table 2: Distribution of parity and number of miscarriages among the infertile women by age group (years) and body mass index.
The highest miscarriage ratio of 1.7:1 was recorded in the oldest age group, followed by miscarriage ratio of 1.5:1 among those aged 41-45 years. Surprisingly, none of the normal weight infertile women who presented with myoma was parous and only 1 (12.0%) of the 8 obese women was parous with a parity of 1. Ratio of miscarriages per woman was minimal (0.4:1) among normal weight infertile women and maximal (1.9:1) among obese women.
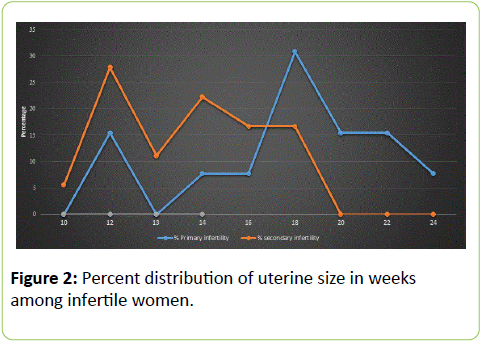
Figure 2 shows the distribution of uterine size (weeks) among the infertile women, indicating that a higher proportion of women with secondary infertility presented with uterine size 10-16 weeks. This situation was reversed as higher proportion of women with primary infertility presented with uterine size 16-24 weeks.
Table 3 showed that a total of 17 (54.8%) patients presented with dysmenorrhea which was more prevalent among women aged 31-35 years (63%), obese women (87%) and those with secondary infertility (56%). Menorrhagia was seen in 14 (45.2%) mostly in all (100%) women aged 26-30 years, those with normal weight (78%) and in primary infertility (54%). In all, 14 (45.2%) infertile women presented with abdominal swelling, seen more frequently among women aged 46-50 years (43%), overweight (50%) and obese (50%) patients and among those with primary infertility (54%). Dysuria, failed IVF and frank abdominal pain were rare clinical presentations.
| Age group (years) | BMI | Infertility | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 26-30 Freq.(%) | 31-35 Freq. (%) | 36-40 Freq. (%) | 41-45 Freq. (%) | 46-50 Freq. (%) | 18.5-24.9 Freq. (%) | 25.0-29.9 Freq. (%) | ≥30 Freq. (%) | Primary Freq. (%) | Secondary Freq. (%) | |
| Symptoms | ||||||||||
| Dysmenorrhea | ||||||||||
| Yes | 2(100) | 5(63) | 6(60.0) | 3(37.0)5(63.0) | 1(33.0)2(67.0) | 6(67.0)3(33.0) | 4(29) | 7(87) | 7(54) | 10(56) |
| No | 0(0) | 3(37) | 4(40.0) | 10(71) | 1(13) | 6(46) | 8(44) | |||
| Abdominal swelling | ||||||||||
| Yes | 1 (50)1 (50) | 3 (37)5 (63) | 6 (60)4 (40) | 2 (25)6 (75) | 2 (67)1 (33) | 3 (33)6 (67) | 7 (50) | 4 (50) | 7 (54) | 7 (39) |
| No | 7 (50) | 4 (50) | 6 (46) | 11 (61) | ||||||
| Abdominal pain | ||||||||||
| Yes | 0 (0) | 1 (13) | 0 (0) | 0 (0) | 0 (0) | 1 (11) | 0 (0) | 0 (0) | 0 (0) | 1 (6) |
| No | 2 (100) | 7 (87) | 10 (100) | 8 (100) | 3 (100) | 8 (89) | 14 (100) | 8 (100) | 13 (100) | 17 (94) |
| Failed IVF | ||||||||||
| Yes | 0 (0)2 (100) | 0 (0)8 (100) | 0 (0)10 (100) | 1 (13)7 (87) | 0 (0)3 (100) | 0 (0)9 (100) | 1 (7)13 (93) | 0 (0)8 (100) | 0 (0.0)13 (100) | 1 (6)17 (94) |
| No | ||||||||||
| Menorrhagia | ||||||||||
| Yes | 2(100)0 (0) | 4 (50)4 (50) | 5 (50)5 (50) | 2 (33)6 (67) | 1 (33)2 (67) | 7 (78)2 (22) | 3 (21)11 (79) | 4 (50)4 (50) | 7 (54)6 (46) | 7 (39)11 (61) |
| No | ||||||||||
| Dysuria | ||||||||||
| Yes | 0 (0)2 (100) | 1 (13)7 (87) | 0 (0)10 (100) | 0 (0)8 (100) | 0 (0)3 (100) | 1 (11)8 (89) | 0 (0)14 (100) | 0 (0)8 (100) | 1 (8)12 (92) | 0 (0)18 (100) |
| No | ||||||||||
| Infertility | ||||||||||
| Yes | 1 (50)1 (50) | 5 (63)3 (37) | 4 (67)2 (33) | 6 (50)6 (50) | 2 (67)1 (33) | 6 (67)3 (33) | 8 (57)6 (43) | 4 (50)4 (50) | 7 (54)6 (46) | 11 (61)7 (39) |
| No | ||||||||||
Table 3: Distribution of symptomatology presented by the infertile women according to age group, BMI and type of infertility. IVF = In Vitro Fertilization; BMI = Body Mass Index.
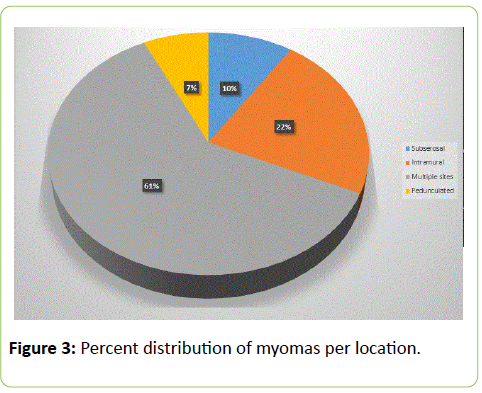
Table 4 shows that the patients’ mean (± sd) uterine size was 15.7 (3.4). Cumulative uterine size was calculated for each age group, BMI and type of infertility and a ratio of uterine size per woman were calculated. Eleven women (35.5%) had uterine size of 16-18 weeks and only 5 (16.1%) women had uterine sizes of 20 weeks and above. The highest ratio of uterine size (in weeks) per infertile woman was observed among those aged 46-50 years (17.3 per woman), among obese infertile women (16.4 per woman) and among those with primary infertility (18.0 per woman). Figure 3 is a graphical illustration of the distribution of percent frequency distribution of myomas among the patients.
| Uterine size (weeks) | Total uterine size (weeks) | Total number of women | Uterinesize/woman | Mean(± sd) uterine size | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 10 | 12 | 13 | 14 | 16 | 18 | 20 | 22 | 24 | - | - | - | - | |
| All | - | - | - | - | - | - | - | - | - | 488 | 31 | 15.7/1 | 15.7(3.6) |
| Age-group | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 25-30 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 34 | 2 | 17.0/1 | 17.0(1.4) |
| 31-35 | 1 | 2 | 1 | 0 | 2 | 0 | 1 | 1 | 0 | 121 | 8 | 15.1/1 | 15.1(4.2) |
| 36-40 | 0 | 2 | 0 | 2 | 0 | 4 | 1 | 0 | 1 | 168 | 10 | 16.8/1 | 16.8(3.8) |
| 41-45 | 0 | 2 | 1 | 3 | 1 | 1 | 0 | 0 | 0 | 113 | 8 | 14.1/1 | 14.1(2.0) |
| 46-50 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 52 | 3 | 17.3/1 | 17.3(5.0) |
| BMI | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Normal | 0 | 3 | 0 | 0 | 2 | 2 | 1 | 1 | 0 | 146 | 9 | 16.2/1 | 16.2(3.7) |
| Overweight | 1 | 2 | 1 | 4 | 2 | 3 | 0 | 1 | 0 | 211 | 14 | 15.1/1 | 15.1(3.1) |
| Obese | 0 | 2 | 1 | 1 | 0 | 2 | 1 | 0 | 1 | 131 | 9 | 16.4/1 | 16.4(4.3) |
| Type of infertility | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Primary | 0 | 2 | 0 | 1 | 1 | 4 | 2 | 2 | 1 | 234 | 13 | 18.0/1 | 18.0(3.7) |
| Secondary | 1 | 5 | 2 | 4 | 3 | 3 | 0 | 0 | 0 | 254 | 18 | 14.1/1 | 14.1(2.4) |
Table 4: Uterine size (weeks) by age-group (years), body mass index (BMI) and type of infertility.
Figure 3 is a graphical illustration of the mean number of myomas observed in each of the four identified sites where the fibroids were found. Most (15, 48.4%) infertile women had their myomas located in multiple sites, with 10 (32.26%) and 4 (12.90%) myomas solely intramural and subserosal respectively. Two (6.45%) fibroids were exclusively pedunculated.
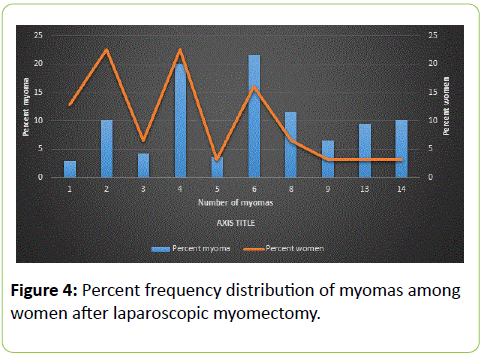
Table 5 shows that 6 seedlings were the most frequent number of fibroid seedlings removed from 5 (16.1%) individual patients, contributing 30 (21.6%) of the total number of fibroids enucleated. This was followed by 4 seedlings removed from 7 (22.6%) individual patients contributing 28 (20.1%) of the enucleated fibroids. The largest number of seedlings removed from a patient was 14 (Figure 4).
| •Absolute number of myomas enucleated | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age group(years) | 1 | 2 | 3 | 4 | 5 | 6 | 8 | 9 | 13 | 14 | Total(%) of myoma enucleated | Total(%) of women |
| 25-30 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 6 (4.3) | 2 (6.5) |
| 31-35 | 0 | 2 | 1 | 3 | 0 | 1 | 1 | 0 | 0 | 0 | 33 (23.7) | 8 (25.8) |
| 36-40 | 2 | 1 | 0 | 2 | 1 | 2 | 0 | 1 | 1 | 0 | 51 (36.7) | 10 (32.3) |
| 41-45 | 2 | 3 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 23 (16.6) | 8 (25.8) |
| 46-50 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 26 (18.7) | 3 (9.7) |
| BMI | ||||||||||||
| Normal | 0 | 2 | 1 | 2 | 0 | 1 | 2 | 1 | 0 | 0 | 46 (33.1) | 9 (29.0) |
| Overweight | 3 | 3 | 1 | 3 | 1 | 3 | 0 | 0 | 0 | 0 | 47 (33.8) | 14 (45.2) |
| Obese | 1 | 2 | 0 | 2 | 0 | 1 | 0 | 0 | 1 | 1 | 46 (33.1) | 8 (25.8) |
| Type of infertility | ||||||||||||
| Primary | 1 | 2 | 0 | 4 | 0 | 2 | 2 | 1 | 1 | 0 | 71 (51.1) | 13 (41.9) |
| Secondary | 3 | 5 | 2 | 3 | 1 | 3 | 0 | 0 | 0 | 1 | 68 (48.9) | 18 (58.1) |
Table 5: Frequency and percent distribution of individual myoma relative to age, body mass index and type of infertility.
Overall, 139 myomas were enucleated from 31 patients, mostly (51, 36.7%) from those aged 36-40 years (10, 32.3%), mostly (47, 33.8%) from overweight women (14, 45.2%) most (71, 51.1%) from women with primary infertility (13, 41.9%).
Table 6 shows that multiport laparoscopy was the sole method used for all the patients, 17 (55%) using 3 ports, 9 (29%) 2 ports and 5 (16%) using 4 ports. Majority (22, 71%) used Palmer’s point of entry. Overall mean (± sd) blood loss was 399 (± 338) ml ranging from 60 to 1,500 mls. There was no significant difference (t = 1.24, p = 0.22) in the immediate mean pre-op (34.7 ± 3.3) and post-op (33.6 ± 3.7) Packed Cell Volume (PCV). Only three (9.7%) patients needed blood transfusion among whom were all who had continuous interlocking closure of myoma bed, two who individually presented with four myomas and one who presented with thirteen myomas; two who presented with uterine size 16 weeks and 1 with uterine size 24 weeks. In all, 7(23.0%) patients developed post-op complications. Complications included one hematoma collection and one excessive hemorrhage of about 1.5 ltrs warranting open laparotomy. The remaining five patients presented with pyrexia that resolved with the administration of simple analgesics. There were no anesthetic complications. There was no evidence of association between previous abdominal surgeries, previous induced abortion, body mass index and the rate of complications.
| Use of Palmer point | No. of accessory ports used | Pre-operation complication | Intra-operation complication | Convert to Laparotomy | Excess blood loss | Pre-op PCV | Post-op PCV | Closure of myoma bed | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes Freq. (%) | No | 2 | 3 | 4 | Yes | No | Yes | No | Yes | No | Mean (±sd) | Mean (±sd) | Mean (±sd) | SF | ED Freq.(%) | CIL | CIC | |
| Freq.(%) | Freq.(%) | Freq.(%) | Freq.(%) | Freq.(%) | Freq.(%) | Freq.(%) | Freq.(%) | Freq.(%) | Freq.(%) | Freq.(%) | Freq.(%) | Freq.(%) | ||||||
| All | 22 (71) | 9 (29) | 9 (29) | 17 (55) | 5 (16) | 1 (5) | 30 (97) | 4 (13) | 27 (87) | 1 (3) | 30 (97) | 399 (338) | 34.7 (3.3) | 33.6 (3.7) | 6 (19) | 1 (3) | 20 (65) | 4 (13) |
| Freq. (%) | ||||||||||||||||||
| Age group | ||||||||||||||||||
| 25-30 | 1 (5) | 1 (11) | 2 (22) | 0 (0) | 0 (0) | 0 (0) | 2 (7) | 0 (0) | 2 (7) | 0 (0) | 2 (7) | 225.0 (35.4) | 32.0 (5.7) | 31.5 (6.4) | 1 (17) | 0 (0) | 1 (5) | 0 (0) |
| 31-35 | 5 (23) | 3 (33) | 2 (22) | 5 (29) | 1 (20) | 1 (100) | 7 (23) | 1 (25) | 7 (26) | 0 (0) | 8 (27) | 312.5 (208.3) | 34.5 (4.0) | 33.5 (3.8) | 1 (17) | 1 (100) | 6 (30) | 0 (0) |
| 36-40 | 5 (23) | 5 (56) | 4 (44) | 6 (35) | 0 (0) | 0 (0) | 10 (33) | 3 (75) | 7 (26) | 1 (100) | 9 (30) | 501.0 (488.9) | 35.1 (3.5) | 33.7 (4.7) | 1 (17) | 0 (0) | 9 (45) | 0 (0) |
| 41-45 | 8 (36) | 0 (0) | 0 (0) | 4 (23) | 4 (80) | 0 (0) | 8 (27) | 0 (0) | 8 (30) | 0 (0) | 8 (27) | 375.0 (291.5) | 34.5 (2.3) | 33.7 (2.4) | 2 (33) | 0 (0) | 3 (15) | 3 (75) |
| 46-50 | 3 (14) | 0 (0) | 1 (11) | 2 (12) | 0 (0) | 0 (0) | 3 (10) | 0 (0) | 3 (11) | 0 (0) | 3 (11) | 466.7 (251.7) | 36.7 (1.5) | 35.2 (1.3) | 1 (17) | 0 (0) | 1 (5) | 1 (25) |
| BMI | ||||||||||||||||||
| Normal | 7 (32) | 2 (22) | 2 (22) | 6 (35) | 1 (20) | 0 (0) | 9 (30) | 1 (25) | 8 (30) | 0 (0) | 9 (30) | 312.2 (242.1) | 34.1 (4.2) | 33.0 (4.2) | 2 (33) | 0 (0) | 6 (30) | 1 (25) |
| Over- | 10 (45) | 4 (44) | 5 (56) | 6 (35) | 3 (60) | 1 (100) | 13 (43) | 1 (25) | 13 (48) | 0 (0) | 14 (47) | 371.4 (286.0) | 34.8 (3.0) | 33.9 (2.9) | 3 (50) | 1 (100) | 8 (40) | 2 (50) |
| Weight | ||||||||||||||||||
| Obese | 5 (23) | 3 (33) | 2 (22) | 5 (29) | 1 (20) | 0 (0) | 8 (27) | 2 (50) | 6 (22) | 1 (100) | 7 (23) | 543.8 (484.4) | 35.4 (3.1) | 34.0 (4.5) | 1 (17) | 0 (0) | 6 (30) | 1 (25) |
| Type of infertility | ||||||||||||||||||
| Primary | 8 (36) | 5 (56) | 5 (56) | 8 (47) | 0 (0) | 0 (0) | 13 (43) | 4 (100) | 9 (33) | 1 (100) | 12 (40) | 496.9 (444.7) | 34.0 (4.0) | 32.4(4.6) | 3 (50) | 0 (0) | 9 (45) | 1 (25) |
| Secondary | 14(64) | 4 (44) | 4 (44) | 9 (53) | 5 (100) | 1(100) | 17 (57) | 0 (0) | 18 (67) | 0 (0) | 18 (60) | 327.8 (221.1) | 35.3 (2.7) | 34.5 (2.6) | 3 (50) | 1 (100) | 11 55) | 3 (75) |
Table 6: Management of operational procedures. PCV = Packed Cell Volume: SF = Stratafix; ED = Electrodiathermy; CIL = Continuous Interlocking; CIC = Continuous Intracorporeal.
Conversion to laparotomy occurred in 1 (3.2%) out of LM performed. Closure of myoma bed was mostly single layer closure (20, 65%). Nine (11%) had multi-layer closure and electro diathermy was used in 1 (3%) of the patients. All fibroids were retrieved by morcellation (139 or 100%).
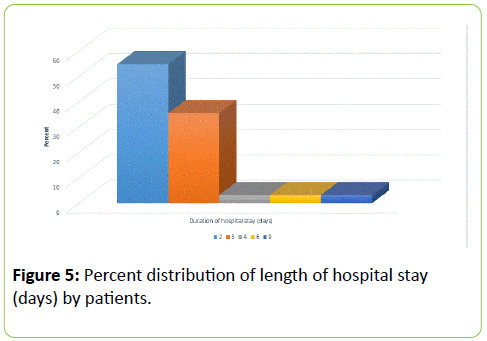
The mean (± sd) length of hospital stay was 2.77 (2.9) days ranging from 2 to 9 days. As illustrated in Figure 5 and Table 7.
| Length of hospital stay(days) | Comorbidity | Post-operation blood transfusion | Pregnancy outcome | Post-operation complication | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean(± sd) | Yes | No | Yes | No | No treatment | Positive | Negative | Treatment not yet started | Yes | No | |
| Freq.(%) | Freq. (%) | Freq. (%) | Freq. (%) | Freq. (%) | Freq. (%) | Freq. (%) | Freq. (%) | Freq. (%) | Freq. (%) | ||
| All | 2.77 (1.43) | 4 (13) | 27 (87) | 3 (9.7) | 28 (90) | 16 (52) | 11 (35) | 3 (10) | 1 (3) | 7 (23) | 24 (77) |
| Age group | |||||||||||
| 25-30 | 2.0 (0.0) | 0 (0) | 2 (7) | 0 (0) | 2 (7) | 2 (13) | 0 (0) | 0 (0) | 0 (0) | 1 (14) | 1 (4) |
| 31-35 | 2.5 (0.5) | 1 (33) | 7 (26) | 1 (33) | 7 (25) | 3 (19) | 4 (36) | 1 (33) | 0 (0) | 1 (14) | 7 (29) |
| 36-40 | 3.6 (2.3) | 1 (33) | 9 (33) | 2 (67) | 8 (28.5) | 6 (37) | 4 (36) | 0 (0) | 0 (0) | 5 (71) | 5 (21) |
| 41-45 | 2.4 (0.5) | 1 (33) | 6 (22) | 0 (0) | 8 (28.5) | 3 (19) | 3 (27) | 1 (33) | 1 (100) | 0 (0) | 8 (33) |
| 46-50 | 2.3 (0.6) | 0 (0) | 3 (11) | 0 (0) | 3 (11) | 2 (12) | 0 (0) | 1 (33) | 0 (0) | 0 (0) | 3 (13) |
| BMI | |||||||||||
| Normal | 2.6 (0.5) | 0 (0) | 9 (33) | 0 (0) | 9 (32) | 7 (44) | 1 (9) | 1 (33) | 0 (0) | 3 (43) | 6 (25) |
| Overweight | 2.7 (1.1) | 3 (75) | 11 (41) | 2 (67) | 12 (43) | 5 (31) | 7 (64) | 1 (33) | 1 (100) | 2 (29) | 12 (50) |
| Obese | 3.1 (2.5) | 1 (25) | 7 (26) | 1 (33) | 7 (25) | 4 (25) | 3 (27) | 1 (33) | 0 (0) | 2 (29) | 6 (25) |
| Type of infertility | |||||||||||
| Primary | 3.1 (2.1) | 0 (0) | 13 (48) | 2 (67) | 11 (39) | 10 (63) | 2 (18) | 1 (33) | 0 (0) | 6 (86) | 7 (29) |
| Secondary | 2.5 (0.6) | 4 (100) | 14 (52) | 1 (33) | 17 (61) | 6 (37) | 9 (82) | 2 (67) | 1 (100) | 1 (14) | 17 (71) |
Table 7: Mean length of hospital stay, outcome of pregnancy and postop management.
14 (45.2%) patients had a hospital stay of 2 days’ duration and another 11 (35.5%) for 3 days’ duration. Twenty-seven (87%) of the patients had no co-morbidities while four (13%) did have, among whom were two with adenomyosis, one with endometriotic deposits and another with adenomyosis and endometriosis.
After having hysteroscopy 8 weeks post LM to check the integrity of the uterine cavity, 15 out of the 31 women went ahead with in-vitro fertilization treatment. Three (20%) of them had live births, 2 with single live births (male and female) and one with twin live birth.
Discussion
Women with primary infertility were more likely to have larger uterine sizes due to fibroids. Even though the debate continues if fibroids are linked to infertility [29,30]. Majority of the women had secondary infertility and were overweight. Dysmenorrhea and menorrhagia followed by abdominal swelling were the common presentations or symptoms in that order. The fibroids were more likely to be in multiple sites. Intramural fibroids were commoner.
The most seedlings were retrieved from women who were overweight and had primary infertility. It is noteworthy that multiple port approach was the main method used and palmer’s point was the point of entry in most of the cases. The complication rate was 26% even though included in this was a case of reaction to blood transfusion. Others included pelvic infection and one hematoma formation. The conversion rate from laparoscopy to laparotomy was 3.2% [1] and it was in the case of a 93.4 kg woman who had a 24-week size uterine mass and 13 fibroids seedlings were retrieved from her. She lost 1500 ml of blood. The conversion rate in this study was similar to 3.4% reported in another study [31] but lower than the 11.3% reported in another study which found the main risk of conversion to be size of myoma, anterior location, intramural fibroids and use of Gonadotropin-releasing hormone (GnRH) agonist pre-operatively [32].
It is important to take myoma size, location and number into consideration to prevent complications needing conversion to open procedure. Three of the 15 women who proceeded to have IVF had live babies delivered by elective caesarean section. This was lower than the 37.9% reported in another study among women who had assisted reproduction post laparoscopic myomectomy [31]. It is important to consider the possibility of other factors affecting outcome of assisted conception. There were no reported uterine ruptures. Similar post laparoscopic myomectomy births with no rupture have been reported in both prospective [33] and retrospective [34] studies. However, caution must be taken in opting for vaginal births especially in cases where the cavity was entered into. Currently, no clear guidelines exist regarding the choice of mode of delivery after myomectomy [31]. The mean blood loss was 442 mls and there was significant difference in mean preoperative and post-operative packed cell volume though only four women needed transfusion. This may be due to the fact that majority of the patients had multiple fibroids. The mean hospital stay was short. This is one of the benefits of laparoscopic myomectomy. A recent meta-analysis showed that laparoscopic myomectomy achieved lower blood loss, post-operative pain and overall complications compared to open myomectomy however operation time was increased in the laparoscopic myomectomy group [35,36].
Conclusion
Laparoscopic myomectomy can be regarded as a safe and beneficial alternative to open myomectomy. However, importance of endoscopic training and proper selection of patients especially in developing countries cannot be overemphasized. A total of 139 fibroids were removed from 31 infertile women before undergoing IVF. These fibroids were more in multiple sites. Multiport laparoscopy was the sole method used for myomectomy among the patients. Overall mean blood loss was 399 mls and only 3 patients required blood transfusion The mean length of hospital stay was 2.77 days and 27 of the patients had no co-morbidities. In all 15 of the 31 infertile women completed IVF treatment among whom 3 gave birth to live babies. It can be concluded that laparoscopic myomectomy, when performed by an experienced surgeon, can be considered a safe technique with an extremely low failure rate and good results in terms of pregnancy outcome.
Recommendation
For women who wish to preserve their uterus after removal of fibroid, myomectomy is a recommended option, though such women need to be counselled on not only the procedure itself but also on the risk of requiring further intervention. The surgeon should consider myomectomy during hysteroscopy as first-line conventional surgical remedy for the management of symptomatic intra-uterine fibroids. The importance of carefully monitor intra-operational fluid balance during removal of fibroids at hysteroscopy, is suggested.
Conflicting of Interest
The authors declare no conflicting interest
References
- Buttram VC Jr, Reiter RC (1981) Uterine leiomyomata: etiology, symptomatology, and management. FertilSteril 36: 433-445.
- Nezhat C, Kho K, Goldfarb H, Seidman D (2015) Laparoscopic Myomectomy. Assessed on15th August
- Cramer SF, Robertson AL Jr, Ziats NP, Pearson OH (1985) Growth potential of human uterine leiomyomas: some in vitro observations and their implications. ObstetGynecol 66: 36-41.
- Trivedi P, Abreo M (2009) Predisposing factors for fibroids and outcome of laparoscopic myomectomy in infertility. J GynecolEndoscSurg 1: 47-56.
- Benecke C, Kruger TF, Siebert TI, Van der Merwe JP, Steyn DW (2005) Effect of fibroids on fertility in patients undergoing assisted reproduction. A structured literature review. GynecolObstet Invest 59: 225-230.
- Donnez J, Jadoul P (2002) What are the implications of myomas on fertility? A need for a debate? Hum Reprod 17: 1424-1430.
- Manyonda I, Sinthamoney E, Belli AM (2004) Controversies and challenges in the modern management of uterine fibroids. BJOG 111: 95-102.
- Practice Committee of the American Society for Reproductive Medicine (2006) Myomas and reproductive function. FertilSteril 86: S194-199.
- Rackow BW, Arici A (2005) Fibroids and in-vitro fertilization: which comes first? CurrOpinObstetGynecol 17: 225-231.
- Fernandez H, Sefrioui O, Virelizier C, Gervaise A, Gomel V, et al. (2001) Hysteroscopic resection of submucosalmyomas in patients with infertility. Hum Reprod 16: 1489-1492.
- Goldenberg M, Sivan E, Sharabi Z, Bider D, Rabinovici J, et al. (1995) Outcome of hysteroscopic resection of submucousmyomas for infertility. FertilSteril 64: 714-716.
- Buttram VC Jr, Reiter RC (1981) Uterine leiomyomata: etiology, symptomatology, and management. FertilSteril 36: 433-445.
- Deligdish L, Loewenthal M (1970) Endometrial changes associated with myomata of the uterus. J ClinPathol 23: 676-680.
- Hunt JE, Wallach EE (1974) Uterine factors in infertility--an overview. ClinObstetGynecol 17: 44-64.
- Vollenhoven BJ, Lawrence AS, Healy DL (1990) Uterine fibroids: a clinical review. Br J ObstetGynaecol 97: 285-298.
- Brady PC, Stanic AK, Styer AK (2013) Uterine fibroids and subfertility: an update on the role of myomectomy. CurrOpinObstetGynecol 25: 255-259.
- Semm K, Mettler L (1980) Technical progress in pelvic surgery via operative laparoscopy. Am J ObstetGynecol 138: 121-127.
- Holub Z (2007) [Laparoscopic myomectomy: indications and limits]. CeskaGynekol 72: 64-68.
- Cittadini E (1998) Laparoscopic myomectomy: the Italian experience. J Am AssocGynecolLaparosc 5: 7-9.
- Stovall DW, Parrish SB, Van Voorhis BJ, Hahn SJ, Sparks AE, et al. (1998) Uterine leiomyomas reduce the efficacy of assisted reproduction cycles: results of a matched follow-up study. Hum Reprod 13: 192-197.
- Dubuisson JB, Chapron C, Chavet X, Gregorakis SS (1996) Fertility after laparoscopic myomectomy of large intramural myomas: preliminary results. Hum Reprod 11: 518-522.
- Sizzi O, Rossetti A, Malzoni M, Minelli L, La Grotta F, et al. (2007) Italian multicenter study on complications of laparoscopic myomectomy. J Minim Invasive Gynecol 14: 453-462.
- Roopnarinesingh S, Suratsingh J, Roopnarinesingh A (1985) The obstetric outcome of patients with previous myomectomy or hysterotomy. West Indian Med J 34: 59-62.
- Goldberg J, Pereira L (2006) Pregnancy outcomes following treatment for fibroids: uterine fibroid embolization versus laparoscopic myomectomy. CurrOpinObstetGynecol 18: 402-406.
- Altgassen C, Kuss S, Berger U, Löning M, Diedrich K, et al. (2006) Complications in laparoscopic myomectomy. SurgEndosc 20: 614-618.
- Holzer A, Jirecek ST, Illievich UM, Huber J, Wenzl RJ (2006) Laparoscopic versus open myomectomy: a double-blind study to evaluate postoperative pain. AnesthAnalg 102: 1480-1484.
- Desai P, Patel P (2011) Fibroids, infertility and laparoscopic myomectomy. J GynecolEndoscSurg 2: 36-42.
- Tsuji I, Ami K, Miyazaki A, Hujinami N, Hoshiai H (2009) Benefit of diagnostic laparoscopy for patients with unexplained infertility and normal hysterosalpingography findings. Tohoku J Exp Med. 219: 39-42.
- Pritts EA, Parker WH, Olive DL (2009) Fibroids and infertility: an updated systematic review of the evidence. FertilSteril 91: 1215-1223.
- Pritts EA (2001) Fibroids and infertility: a systematic review of the evidence. ObstetGynecolSurv 56: 483-491.
- Lourens RJ, Siebert TI, Kruger TF, Van der Merwe JP (2011) Laparoscopic myomectomy for infertile women with intramural fibroids: A retrospective study at a tertiary endoscopic centre. SAJOG Vol. 17 No. 3.
- Sinha R, Hegde A, Mahajan C, Dubey N, Sundaram M (2008) Laparoscopic myomectomy: do size, number, and location of the myomas form limiting factors for laparoscopic myomectomy? J Minim Invasive Gynecol 15: 292-300.
- Kumakiri J, Takeuchi H, Itoh S, Kitade M, Kikuchi I, et al. (2008) Prospective evaluation for the feasibility and safety of vaginal birth after laparoscopic myomectomy. J Minim Invasive Gynecol 15: 420-424.
- Seracchioli R, Manuzzi L, Vianello F, Gualerzi B, Savelli L, et al. (2006) Obstetric and delivery outcome of pregnancies achieved after laparoscopic myomectomy. FertilSteril 86: 159-165.
- Jin C, Hu Y, Chen XC, Zheng FY, Lin F, et al. (2009) Laparoscopic versus open myomectomy--a meta-analysis of randomized controlled trials. Eur J ObstetGynecolReprodBiol 145: 14-21.
- Lefebvre G, Vilos G, Allaire C, Jeffrey J, ArnejaJ,et al. (2003) Clinical Practice Gynaecology Committee, Society for Obstetricians and Gynaecologists of Canada. The management of uterine leiomyomas. ObstetGyn

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences