Long Term Effect of Physiotherapeutic Intervention on BCRL-A Case Report
Bhavna Anand1, Ruchika Kalra2* and Harshita Sharma3
1Teaching Associate, BPT, MPT, PhD Scholar, Amity Institute of physiotherapy, Amity University Noida, Uttar Pradesh, India
2Physiotherapist, BPT, Amity Institute of physiotherapy, Amity University Noida, Uttar Pradesh, India
3Consultant Physiotherapist, BPT, MPT, MBA, MAX Super Speciality Hospital, Delhi, India
- *Corresponding Author:
- Ruchika Kalra
Physiotherapist, BPT, Amity Institute of physiotherapy, Amity University Noida, Uttar Pradesh, India
E-mail: kalraruchika123@gmail.com
Received Date: July 02, 2021; Accepted Date: July 16, 2021; Published Date: July 23, 2021
Citation: Anand B, Kalra R, Sharma H (2021) Long Term Effect of Physiotherapeutic Intervention on BCRL-A Case Report. Med Clin Rev Vol.7 No.7:144.
Abstract
Introduction: BCRL is commonest complication arriving after the breast cancer treatment, can be complicated if not managed and prevented early. This case study presents the BCRL at later stage and been resolved with long term intervention.
Patient concerns: A 67-year-old woman presented with heaviness and increase size of the left arm and is progressive in the last 8 months and is a left breast cancer survivor.
Diagnosis: She was diagnosed with BCRL which was diagnosed on the basis of her increased circumferential measurements and breast cancer history with axillary lymph node dissection.
Interventions: The patient was provided with the CDT a gold standard treatment for lymphedema with IPC and resistance exercises training as the progression with later stages in addition in exercise therapy.
Result: Patient followed the treatment for 70 days and resulted in decreased stage from 3 to 1 and enhancer muscular power and decreased circumferential measurements.
Conclusion: BCRL is the complication which requires the prevention and management as early as possible. The BCRL is only managed and not cured so prevention measures required even after resolved and reoccurrence is possible.
Abbreviations: BCRL- Breast cancer related lymphedema, VAS- Visual analogue scale, CDT-Complex decongestive therapy, IPC- Intermittent pneumatic compression, AROM-Active range of motion, LT UL-Left upper limb, RT UL- Right upper limb.
Keywords
Resistance training; Breast cancer
Introduction
The breast cancer is one of the commonest cancers in women where the life expectancy is quite higher as the basic treatment following with chemotherapy, radiotherapy and surgery [1]. These treatments enhance life expectancy but affect the quality of life as leading to different complications such as Breast cancer related lymphedema (BCRL) [2]. BCRL is complication that arrives due to treatment effects such as removal of axillary lymph nodes, radiation leading to scarring of the lymph nodes and so on [3]. In BCRL the affected arm presents with the accumulation of lymphatic fluid which can be accumulated in alternated nodes or complete arm or even on the breast tissue if the lumpectomy is performed but it duly depends on the removal of the number of lymph nodes [4, 5]. Lymphedema presents with signs of heaviness in the arm, decreased range of motion, circumferential increase in the affected arm, numbness in the arm, decreased muscle power [6-8]. According to the studies there are various assessment tools for measuring the lymphedema by circumference, water displacement method, infrared perometry and bioelectrical impedance having different approach towards measuring size to change in limb volume [9].
Studies presenting various treatments for the BCRL having positive results in significant reduction in lymphedema but CDT came to be the gold standard treatment for the BCRL patients even in there later and permanent stages of lymphedema and present with promising results so as the case presented below [10, 11]. The patient was informed for data extraction and her consent was shared with our team for publication.
Case Presentation
A 67-year-old female patient weighing 70 kg (endomorphic) and height of 147.8cm presented with the chief complaint of swelling in the left upper limb in the last 8 months and was progressive. The patient complaint of heaviness, increased in the size of the limb; the pain and heaviness on the surgical area. The assessment of the patient started for the medical history where she was the breast cancer survivor at the stage 2 and had got modified radical mastectomy with axillary lymph node dissection last year followed with radiation of 18 cycles and prior mastectomy had 21 cycles of chemotherapy. The patient was presented with a comorbidity of hypothyroidism for last 5 years and a hysterectomy 3 years ago.
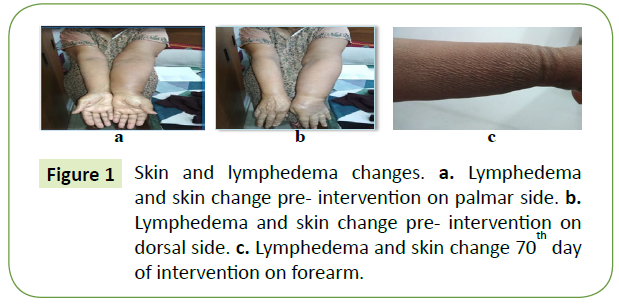
Patient was observed on stage of lymphedema [12] where she was diagnosed at the stage 3 with the fibrosis of the skin with oedema specially in the forearm and the dorsal area of hand (Figure 1). The lymphedema was measured with the help of circumference from the palm to tip of shoulder, by keeping the gap of 4 cm apart from wrist to tip of shoulder and measuring the circumference in the centimeters for bilateral upper limb; the measurements were having a great difference present (Table 1).
| Measurements for the upper limb | Pre intervention | 70th day of follow up | ||
|---|---|---|---|---|
| LT UL | RT UL | LT UL | RT UL | |
| (In cm) | (In cm) | (In cm) | (In cm) | |
| Tip of the Shoulder | 46.8 | 35.5 | 36.1 | 35.6 |
| 4 cm below from above | 46.0 | 35.4 | 35.9 | 35.4 |
| 4 cm below from above | 44.8 | 33.8 | 34 | 33.8 |
| 4 cm below from above | 41.4 | 32.5 | 33 | 32.6 |
| 4 cm below from above | 38.8 | 30.5 | 30.9 | 30.5 |
| 4 cm below from above | 39.5 | 31.4 | 31.9 | 31.5 |
| 4 cm below from above | 36.2 | 29.3 | 29.8 | 29.3 |
| 4 cm below from above | 32.8 | 26.7 | 26.9 | 26.7 |
| 4 cm below from above | 28.7 | 22.4 | 22.7 | 22.6 |
| At Wrist joint | 22.7 | 17.9 | 18.1 | 17.9 |
| At palm to dorsum | 21.9 | 15.8 | 16 | 15.8 |
Table 1: Measurements of upper limb - Presenting the circumferential measurements of the affected and unaffected limb for both pre -intervention and 70th day of follow up.
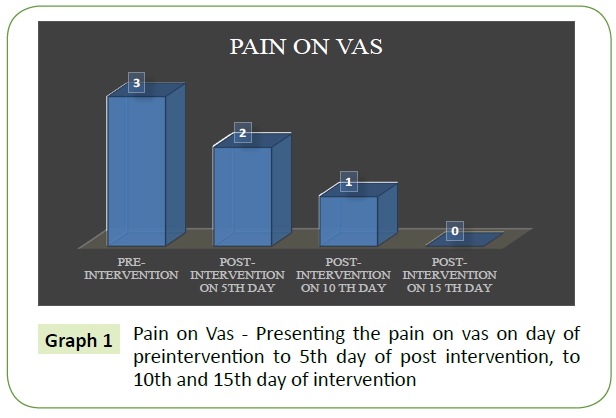
Patient presented with the pain on the VAS scale of 3 out of 10 (Graph 1), on the surgical site as accumulation of lymphatic fluid was observed in the lower segment of the surgical line. The skin changes were firm in nature and with the scar present at the surgical line. The sensory assessment was done to check on the numbness factor present generally in the BCRL patients where it came to be negative as the dermatome examination was intact for the affected and non-affected arm. The manual muscle testing was done for bilateral upper limb group of muscles such as the flexors, extensors, abductors, rotators for shoulder complex which was comparatively less as compared with non- affected shoulder complex so as followed for the elbow complex flexors and extensors, forearm pronators and supinators, and wrist joint flexors, extensors, ulnar deviators and radial deviators comparing for both the upper limb as demonstrated (Table 2).
| MMT for the Upper limb | Pre intervention | 70th day of follow up | ||
|---|---|---|---|---|
| Joint complex - Muscle groups | LT UL | RT UL | LT UL | RT UL |
| Shoulder Joint complex- | ||||
| Flexors | 2+ | 4 | 4 | 4 |
| Extensors | 2+ | 4 | 4 | 4 |
| Abductors | 2+ | 4 | 4 | 4 |
| Adductors | 3 | 4 | 3+ | 4 |
| External rotators | 2 | 4 | 4 | 4 |
| Internal rotators | 2 | 4 | 4 | 4 |
| Elbow joint | ||||
| Flexors | 2+ | 4 | 4 | 4 |
| Extensors | 2+ | 4 | 4 | 4 |
| Radio ulnar joint | ||||
| Pronators | 2+ | 4 | 4 | 4 |
| Supinators | 2+ | 4 | 4 | 4 |
| Wrist joint | ||||
| Flexors | 2+ | 4 | 4 | 4 |
| Extensors | 2+ | 4 | 4 | 4 |
| Radial Deviators | 2+ | 4 | 4 | 4 |
| Ulnar Deviators | 2+ | 4 | 4 | 4 |
Table 2: Manual Muscle Testing of Upper Limb - Presenting the manual muscle testing of the affected and unaffected upper limb for both pre-intervention and 70th day of follow up.
The range of motion was than analyzed with the help of goniometer and the ranges were presented for every range of motion from shoulder to wrist and the motion in all the planes. The range of motion was not that affected and was almost within normal limit of the joint motion (Table 3).
ROM for the Upper limb |
Pre intervention | 70th day of follow up | ||
|---|---|---|---|---|
| (AROM) | (AROM) | |||
| Joint complex and motion | LT UL | RT UL | LT UL | RT UL |
| Shoulder Joint complex | ||||
| Flexion | 0-175° | 0-178˚ | 0-178˚ | 0-180˚ |
| Extension | 0-60˚ | 0-60˚ | 0-60˚ | 0-60˚ |
| Abduction | 0-180˚ | 0-180˚ | 0-180˚ | 0-180˚ |
| External rotation | 0-85 ˚ | 0-85˚ | 0-85˚ | 0-85˚ |
| Internal rotation | 0-85˚ | 0-85˚ | 0-85˚ | 0-85˚ |
| Elbow joint | ||||
| Flexion | 0-140 ˚ | 0-145 ˚ | 0-143 ˚ | 0-145 ˚ |
| Extension | 140-0 ˚ | 145-0 ˚ | 143-0˚ | 145-0 ˚ |
| Radio ulnar joint | ||||
| Pronation | 0-70 ˚ | 0-70 ˚ | 0-70 ˚ | 0-70 ˚ |
| Supination | 0-82 ˚ | 0-82 ˚ | 0-82 ˚ | 0-82 ˚ |
| Wrist joint | ||||
| Flexion | 0-75 ˚ | 0-75 ˚ | 0-75 ˚ | 0-75 ˚ |
| Extension | 0-70 ˚ | 0-70 ˚ | 0-70 ˚ | 0-70 ˚ |
| Radial Deviation | 0-20 ˚ | 0-20 ˚ | 0-20 ˚ | 0-20 ˚ |
| Ulnar Deviation | 0-33 ˚ | 0-33 ˚ | 0-33 ˚ | 0-33 ˚ |
Table 3: Range of motion of upper limb - Presenting the range of motion of the affected and unaffected upper limb for both pre -intervention and 70th day of follow up.
Interventions
The intervention protocol was defined as with the help of the most effectful treatment followed for the BCRL that is combination of the complex decongestive therapy with the combination of the intermittent pneumatic compression. The treatment procedure was followed with division of CDT to manual lymphatic drainage, therapeutic exercises and multi-layer bandaging. The total treatment protocol was followed for 40 minutes intermittent pneumatic compression with 35 minutes of the MLD, 25 minutes of the therapeutic exercises and followed with multi-layer bandaging. The follow up was for 70 days having 6 days a week.
The steps were followed for the manual lymphatic drainage where it was further divided into the Lymph node activation which was stretch and release of 10 cycles to the anatomical areas starting from posterior auricular lymph nodes of bilateral side to supraclavicular lymph nodes of bilateral side to right breast lymph nodes to right axillary lymph nodes just below xiphisternum followed with deep breathing exercises for abdominal lymph nodes and Inguinal lymph nodes. The MLD was continued with manual lymphatic massage where the procedure was 10 circles each to the compartments divided where the superficial massage was provided and drainage to active lymph nodes according to division of arm and chest area segmentally; medial upper quadrant of left chest to right breast to lateral upper quadrant of left breast to left auricular and supraclavicular area to medial lower quadrant of left breast to sternal and abdominal area lateral lower quadrant of left breast to left inguinal and abdominal lymph nodes. to upper arm to auricular and supraclavicular of left side to lower arm to auricular and supraclavicular of left side to at elbow to auricular and supraclavicular of left side to upper forearm to auricular and supraclavicular of left side to at wrist to auricular and supraclavicular of left side to palm and dorsum and fingers to auricular and supraclavicular of left side. The procedure was done in supine lying and side lying. Intermittent pneumatic compression: Applied for 40 minutes on left arm covering chest area at the pressure of 45 MMHG for 20% gradient for lymphedema.
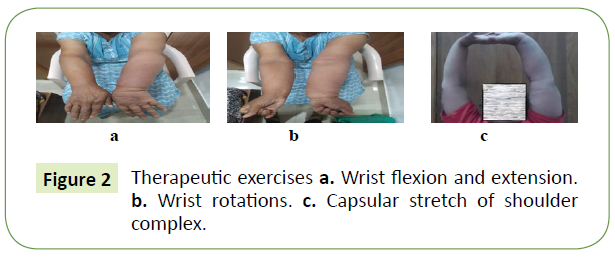
Exercises followed as for left arm followed for 10 repetitions each exercise inclusive of all the range of motion exercises inclusive (Figure 2) of wrist rotations, fanning of fingers, gripping of wrist in flexion at 90, 180 and abduction of shoulder at 90 degrees without resistance, stretch for flexors and extensors of wrist, shoulder rotations, shoulder shrugs, pectoralis stretches, deltoid stretch, triceps stretch and finger ladder in frontal and sagittal plane. The exercises were progressed with the decrease in the lymphedema and increase in the patient’s muscle performance. The progression was with addition of exercises such as wall pushups, gripping exercises with the stress ball, increase in sets from one to 3 sets with each of 10 repetitions. The progression after the successful decrease in the lymphedema helped in the addition of the resistance training with the help of half kilogram weight which included all the range of motion exercises with it as present above with 10 repetitions for first few days progressed with 2 sets. The progression was well kept with the patient consent and will power and initiated with one kilogram weight for range of motion exercises for 2 sets.
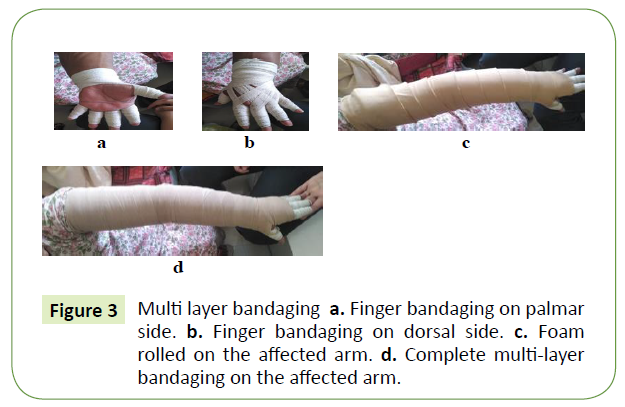
Multi-layer bandaging was followed for each day and wore after the completion of the treatment and removed after 20 hours. The method followed for the wearing of the multilayer bandaging was that finger bandaging covering from wrist to fingers to wrist then arm stockinette then Foam layer in tubular manner then 3 layers of bandaging with no. followed as 1st bandage from wrist to dorsum to palm to wrist in figure of 8 to mid-forearm followed by 2nd bandage from wrist to above in figure of 8 followed by 3rd bandage from where 1st ended followed by 4th bandage from where 2nd ended to tip of shoulder in figure of 8 (Figure 3).
Results
The case was provided with 6 days a week protocol here provided with 40 minutes of intermittent pneumatic compression, 35 minutes of manual lymphatic drainage, 25 minutes of exercises and 10 minutes for multi-layer bandaging. Short term goal was to manage the lymphedema and reduce it, whereas the long-term goal was to enhance the muscle power so as to prevent the progression further. The 70 day follow up came up with accomplishment for both the goals where outcome measures such as circumferential measurement so as the stage of lymphedema which was reduced by 2 stages and enhancement of the muscle power from 2 to 4+ as recorded from pre-intervention to every week to 70th day of follow up. Patient was improving after every week and addition of ease in activities of daily living encouraged her for the daily progression of therapy.
Discussion
This case study explains the management of the BCRL patient present with exaggerated stage of lymphedema that is stage 3 present with fibrotic changes of the skin and non-pitting oedema. There are various studies explaining types of different physiotherapeutic intervention as significant depending on their entitled outcome measures, such as quality of life, circumferential difference, strength of the muscle, lymphatic fluid exchange, decrease in pain in affected limb as on VAS and so on [13]. The outcome measured varies from each study with different sample size, cases and review studies. The quality of life in cancer patients is highly mandatory whenever dealing with the rehabilitation so as to keep the patient confident and self-belief that he or she is improving every day so that they can reach back to their working life as they were [14].
There were various physiotherapeutic interventions such as kinesio taping, compression bandaging, low level laser therapy, manual lymphatic drainage, intermittent pneumatic compression, compression sleeves, exercises varying from aerobic to resistance and complex decongestive therapy. There are studies that have proven that gold standard treatment for the lymphedema treatment is CDT, so as this study was followed with the later staged BCRL and fibrosed condition [15].
The studies have presented that intermittent pneumatic compression plays a role in BCRL reduction but not significantly when utilized alone but better in the combination of the CDT to reduce high grade lymphedema followed in this case study [16, 17].
Resistance exercises can worsen the condition of the BCRL but the studies have proven this statement as myth that resistance exercises do not have any impact on BCRL as some studies have proven that reduction in BCRL is resulted where some have resulted the better muscle outcome allowing the muscle contraction channelizes the lymphatic fluid [18,19].
Conclusion
The case report highlights that the management of the BCRL patient with CDT and IPC followed with progression of resistance training, further leading to promising results in both circumferential measurements, skin changes, decrease in pain on VAS and muscle power. Also, it states that the BCRL should be managed early so as to avoid complications occurring such as permanent fibrotic changes, as well as better functional status and quality of life.
Acknowledgements
We are really thankful for our patient consent for the publication.
Competing interests
No competing interests are there
Funding
There is no funding involved for manuscript.
References
- Winters S, Martin C, Murphy D, Shokar NK (2017) Breast Cancer Epidemiology, Prevention, and Screening. Prog Mol Biol Transl Sci 151: 1-32.
- Paskett ED, Naughton MJ, Mc Coy TP, Case LD, Abbott JM (2007) The epidemiology of arm and hand swelling in premenopausal breast cancer survivors. Cancer Epidem Biomar 16(4): 775-782.
- Shah C, Vicini FA (2011) Breast cancer-related arm lymphedema: incidence rates, diagnostic techniques, optimal management and risk reduction strategies. Int J Radiat Oncol Biol Phys 81(4): 907-914.
- Lawenda BD, Mondry TE, Johnstone PA (2009) Lymphedema: A primerm on the identification and management of a chronic condition in oncologic treatment. CA Cancer J Clin 59(1): 8-24.
- McLaughlin SA, Bagaria S, Gibson T, Arnold M, et al., (2013) Trends in risk reduction practices for the prevention of lymphedema in the first 12 months after breast cancer surgery. J Am Coll Surg 216(3): 380-389.
- Lee BB, Andrade M, Antignani PL, Boccardo F, Bunke N, et al., (2013) Diagnosis and treatment of primary lymphedema. Consensus document of the International Union of Phlebology (IUP). Int Angiol 32(6): 541-74.
- Fu MR, Cleland CM, Guth AA, Kayal M, Haber J, et al., (2013) L-dex ratio in detecting breast cancer-related lymphedema: reliability, sensitivity, and specificity. Lymphology 46(2): 85.
- Fu M, Cleland CM, Guth AA, Qiu Z, Haber J, et al., (2014) The role of symptom report in detecting and diagnosing breast cancer-related lymphedema. European J Clin Med Oncol.
- Armer JM, Stewart BR (2005) A comparison of four diagnostic criteria for lymphedema in a post-breast cancer population. Lymphat Res Biol 3(4): 208-217.
- Yesil H, Eyigör S, Caramat İ, Işık R (2017) Effects of complex decongestive therapy on quality of life, depression, neuropathic pain, and fatigue in women with breast cancer-related lymphedema. Turk J Phys Med Rehabil 63(4): 329.
- Michopoulos E, Papathanasiou G, Vasilopoulos G, Polikandrioti M, Dimakakos E (2020) Effectiveness and Safety of Complete Decongestive Therapy of Phase I: A Lymphedema Treatment Study in the Greek Population. Cureus 12(7): e9264.
- Greene AK, Goss J A (2018) Diagnosis and Staging of Lymphedema. Seminars in plastic surgery 32(1): 12–16.
- Kalra R, Anand B, Shree S, Chauhan, Sharma H (2021) Association of physical activity and quality of life among cancer patients. Int J Med Sci Clin Invent 8(6): 5463-5468.
- Chung C, Lee S, Hwang S, Park E (2013) Systematic review of exercise effects on health outcomes in women with breast cancer. Asian Nurs Res. 7(3): 149-159.
- Anand B, Kalra R, Sharma H (2021) Physiotherapeutic Interventions for Breast Cancer Related Lymphedema in Women: A Review Study. Angiol 9: 126.
- Anand B, Kalra R, Sharma H (2020) Effect of CDT and IPC in Secondary Upper Extremity Lymphedema in Women Post Breast Cancer Surgery on Anxiety, Depression and Quality of Life. 14(4): 211.
- Szolnoky G, Lakatos B, Keskeny T, Varga E, Varga M, et al., (2009) Intermittent pneumatic compression acts synergistically with manual lymphatic drainage in complex decongestive physiotherapy for breast cancer treatment-related lymphedema. Lymphology 42(4): 188-194.
- Chung C, Lee S, Hwang S, Park E (2013) Systematic review of exercise effects on health outcomes in women with breast cancer. Asian Nurs Res 7(3): 149-59.
- Wanchai A, Armer JM (2019) Effects of weight-lifting or resistance exercise on breast cancer-related lymphedema: a systematic review. International journal of nursing sciences 6(1): 92-98.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences