Pathogenesis of Atherosclerosis A Review
Aziz M and Yadav KS
DOI10.21767/2471-299X.1000031
1 Pri-Med Care, Lewisville, Texas 75067, USA
2 Principal, RGCP, Bhopal, India
- *Corresponding Author:
- Maria Aziz
Director, Pri-Med Care
Lewisville, Texas 75067, USA
Tel: 9723656942
E-mail: mariz1979@yahoo.in
Received date: August 05, 2016; Accepted date: August 22, 2016; Published date: August 29, 2016
Citation: Aziz M, Yadav KS. Pathogenesis of Atherosclerosis. Med Clin Rev. 2016, 2:22. doi: 10.21767/2471-299X.1000031
Copyright: ©2016 Aziz M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
In this review, we would discuss the chief pathways involved in the pathophysiology of atherosclerosis. We would also highlight the end terminal events of this sequel with due consideration to risk factors, clinical features, diagnosis and treatment. The aim of the review is to get into the fine details of all possible causes and pathophysiologic mechanisms responsible for atherosclerosis so that new treatment modalities can emerge and reduce the morbidity and mortality associated with atherosclerosis.
Introduction
Atherosclerosis has been derived from a Greek word, Athero meaning gruel [1]. Marchand introduced the term “atherosclerosis” describing the assosciation of fatty degeneration and vessel stiffening [2]. It’s the patchy intramural thickening of the subintima. The earliest lesion is the fatty streak. Fatty streak evolve to fibrous plaque and unstable plaque are responsible for clinical events.
Atherosclerosis is marked by atheromas, patchy intimal plaques. Most common location is lumen of medium sized and large arteries. The plaque has cellular component -namely of inflammatory cells, smooth muscle cells, a fibrous component of –connective tissue and a fat component of lipids. Prominent risk factors of consideration are Hypertension, Diabetes, Dyslipidemia, obesity, sedentary life style, Family history, smoking. Intraplaque rupture, bleeding, thrombosis and stenosis cause symptoms. Diagnosis is clinical and definitive diagnosis is made through Imaging tests. Management plan includes behavior modifications (Physical activity with low caloric diet, rich in fiber component) and main class of drugs used in treatment are antiplatelet drugs and antiatherogenic drugs.
It is the leading cause of morbidity and mortality in the US and western world. In the current era cardiovascular disease (CVD) remains the MCC of death all over the world. In 2008, 17 million deaths were recorded from CVD. More than 3 million of these deaths occurred in people below the age of 60 and could have largely been prevented [3]. There are growing inequalities in the occurrence and outcome of CVD between countries and social classes.
Discussion
We would discuss the chief pathways involved in the pathophysiology of atherosclerosis. We would also highlight the end terminal events of this sequel with due consideration to risk factors, clinical features, diagnosis and treatment.
Pathophysiology
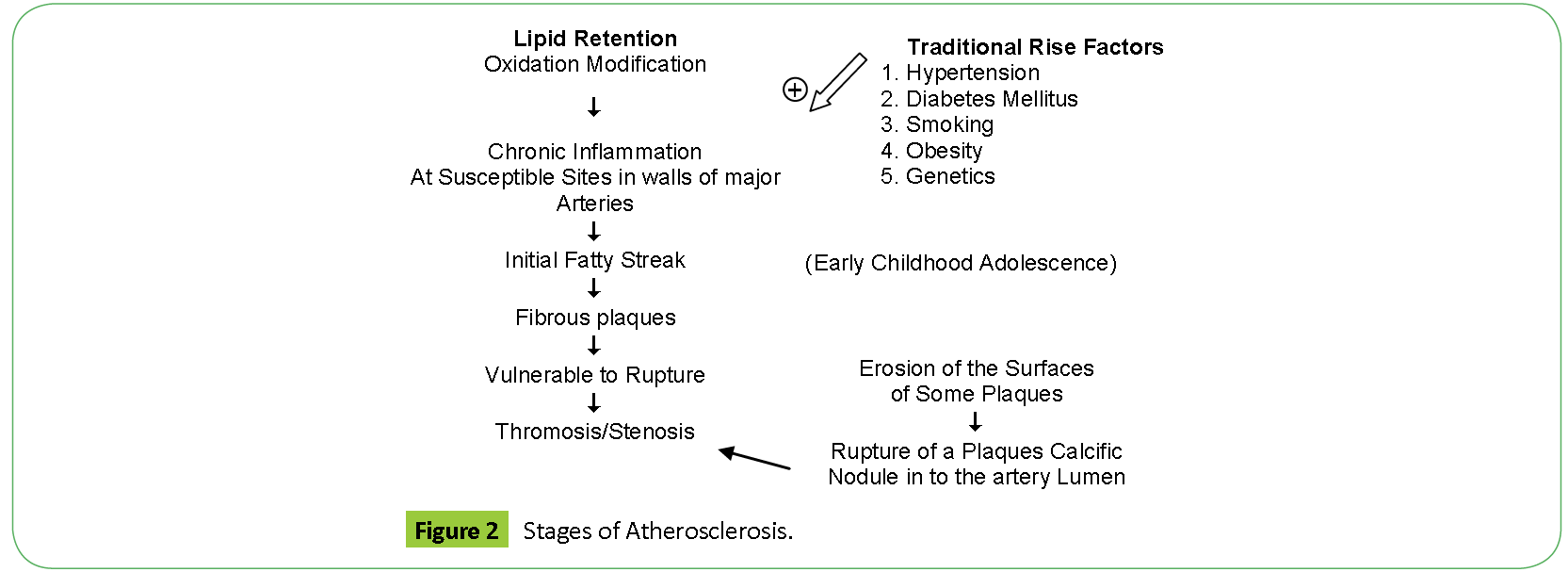
Atherosclerosis is a chronic inflammatory disease. Atherosclerosis begins with fatty streak which is a accumulation of lipid laden foam cells in the intimal layer of the artery [4]. Lipid retention is the first step in the pathogenesis of atherosclerosis which is followed by chronic inflammation at susceptible sites in the walls of the major arteries lead to fatty streaks, which then progress to fibroatheromas which are fibrous in nature (Table 1) [5,6].
| Description | Thrombosis | |
|---|---|---|
| Nonatherosclerotic intimal lesions | ||
| Intimal thickening | Normal accumulation of smooth muscle cells (SMCs) in the intima in the absence of lipid or macrophage foam cells. | Absent |
| Intimal xanthoma | Superficial accumulation of foam cells without a necrotic core or fibrous cap; based on animal and human data, such lesions usually regress. | Absent |
| Progressive atherosclerotic lesions | ||
| Pathologic intimal thickening | SMC-rich plaque with proteoglycan matrix and focal accumulation of extracellular lipid | Absent |
| Fibrous cap atheroma | Early necrosis: focal macrophage infiltration into areas of lipid pools with an overlying fibrous capLate necrosis: loss of matrix and extensive cellular debris with an overlying fibrous cap. | Absent |
| Thin cap fibroatheroma | A thin, fibrous cap (< 65 µm) infiltrated by macrophages and lymphocytes with rare or absence of SMCs and a relatively large underlying necrotic core; intraplaque hemorrhage/fibrin may be present. | Absent |
| Lesions with acute thrombi | ||
| Plaque rupture | Fibroatheroma with fibrous cap disruption; the luminal thrombus communicates with the underlying necrotic core | Occlusive or nonocclusive |
| Plaque erosion | Plaque composition, as above; no communication of the thrombus with the necrotic core; can occur on a plaque substrate of pathologic intimal thickening or fibroatheroma | Usually nonocclusive |
| Calcified nodule | Eruptive (shedding) of calcified nodules with an underlying fibrocalcific plaque with minimal or absence of necrosis | Usually nonocclusive |
| Lesions with healed thrombi | ||
| Fibrotic (without calcification) Fibrocalcific (+/- necrotic core) | Collagen-rich plaque with significant luminal stenosis; lesions may contain large areas of calcification with few inflammatory cells and minimal or absence of necrosis; these lesions may represent healed erosions or ruptures | Absent |
Table 1: Stages of Atherosclerosis: Modified AHA consensus classification based on morphologic descriptions.
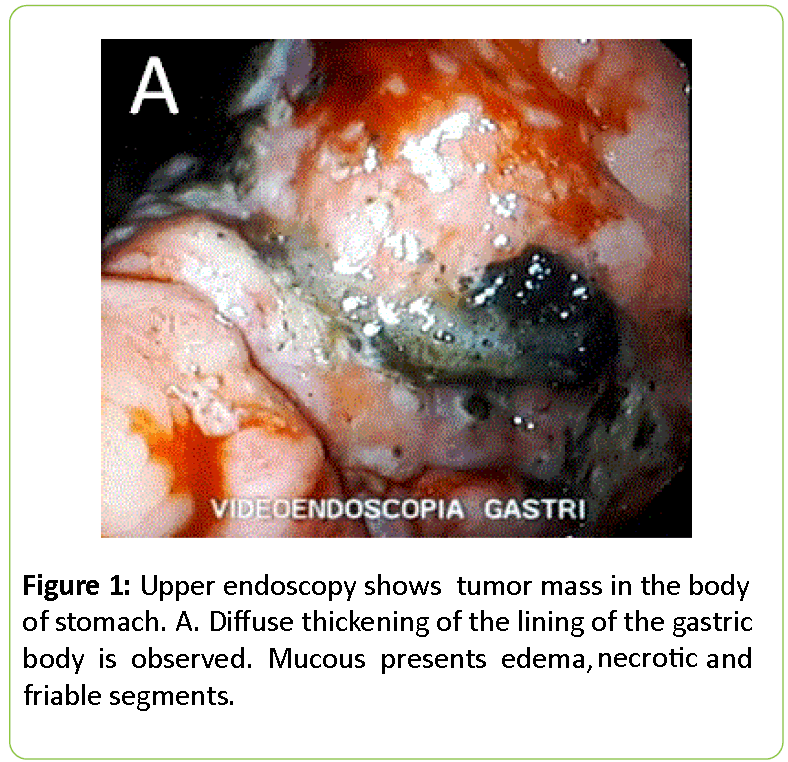
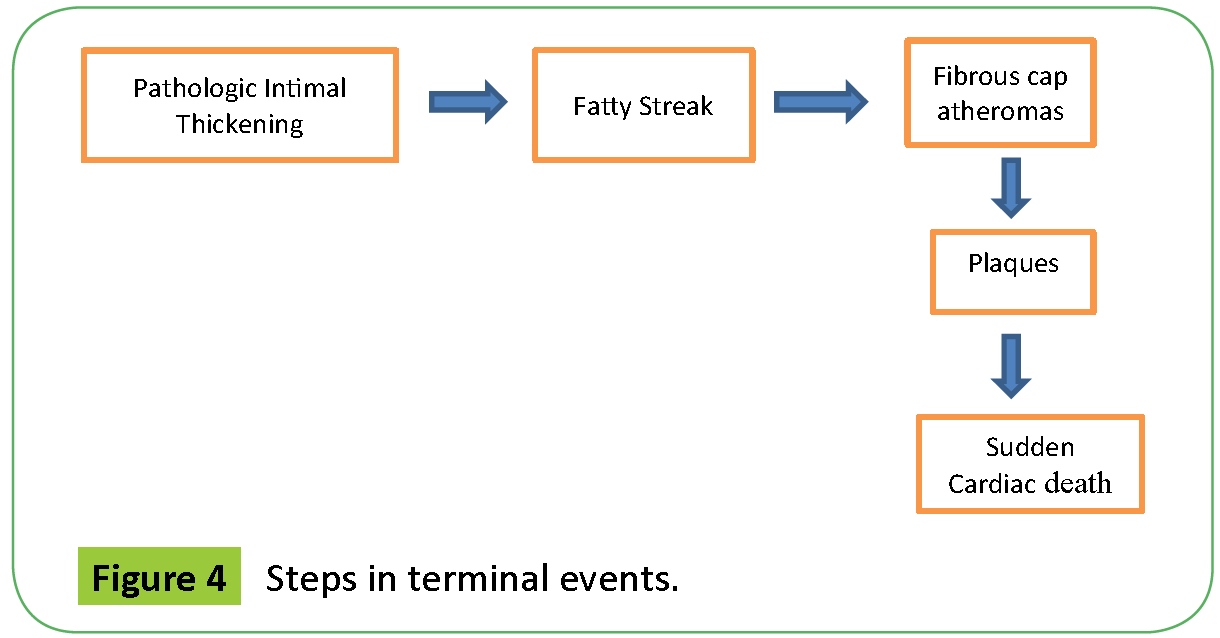
Atherosclerosis is a continuous progressive development. Fatty streak develop at 11-12 years and fibrous plaques at 15-30 years (Figure 1, depicts the conversion of Fatty Streak to Fibrous Plaques) [7] and they develop at the same anatomic sites as the fatty streaks making it more evident that fibrous plaques arise from fatty streak. Pathologic intimal thickening leads to fatty streak, leads to fibrous cap atheromas, lead to plaques, finally leading to sudden cardiac death [8,9].
Fatty streaks evolve to atherosclerotic plaques which is composed of three components namely of inflammatory cells, smooth muscle cells, a fibrous component of–connective tissue and a Fat component of lipids [10].
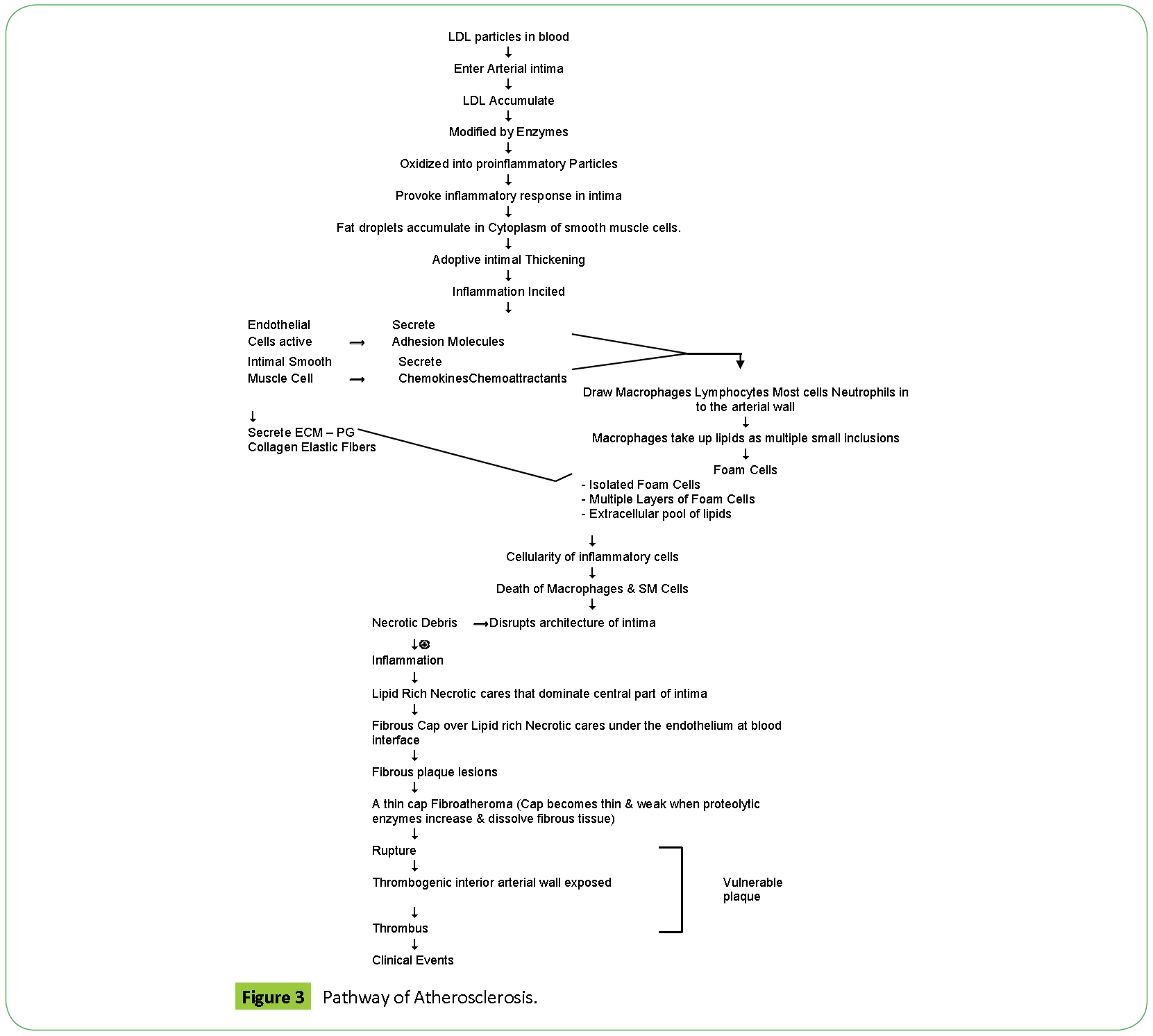
Endothelial Injury plays the inciting role. Turbulent blood flow leads to endothelial dysfunction, it inhibits production of NO, a potent vasodilator and stimulates production of adhesion molecules which attract inflammatory cells. Other risk factors also contribute to this step. The net result is Monocytes and T cells bind to the endothelial cells and migrate to the subendothelial space. Lipids in the blood, LDL, VLDL bind to endothelial cells and oxidize in the subendothelial space. Monocytes in subendothelial space engulf oxidized LDL and transform to foam cells. This mark the first stage i.e., fatty streak. Macrophages further elaborate proinflammatory cytokines which recruit smooth muscle cells. There is smooth muscle cell replication and increase in dense extracellular matrix. End result lesion is a subendothelial fibrous plaque composed of lipid core surrounded by smooth muscle cells and connective tissue fibers (Figures 2 and 3) [11].
There is sequential involvement of arterial layers, intima, then media and finally adventitia. Arterial wall lesions have a central cholesterol rich lipid core surrounded by inflammatory response. Every lesion has lipid accumulation and inflammation. Plaque distorts media/adventitia, increases caliber of arterial lumen and decreases its size simultaneously. New Vasa Vasorum invade diseased intima, cause hemorrhage within arterial wall, leading to intramural hemorrhage and increased fibrous tissue. Rupture of thin fibrous caps leads to thrombosis and healing. Cyclic healing of clinically silent ruptures leads to multiple layer of healed tissue and the end result is sudden cardiac death. Calcium deposits as small aggregates convert later to large nodules in the wall. Erosion of endothelium leads to thrombosis. Increase plaque mass causes stenosis and finally leading to lethal ischemia [12].
There are two types of plaques stable and unstable [13]. Stable plaques regress or are static or they grow slowly. Unstables plaques are complicated by erosion, fissure, rupture and cause stenosis, thrombosis, infarction. Most clinical events result from complications of unstable plaque, hence plaque stabilization can reduce morbidity and mortality associated with atherosclerosis.
Plaque is ruptured by enzymes secreted by activated macrophages in the plaque. Once plaque ruptures, plaque contents get exposed to circulating blood and the end result is thrombosis [14]. The resultant thrombosis may change plaque shape, occlude lumen of blood vessel, may embolise or the plaque contents may embolise. Low risk plaques are more fibrous in content and have low lipids and do not cause 100% blockade while unstable plaques have thick lipid core and thin fibrous cap narrow lumen <50% and tend to rupture unpredictably [15].
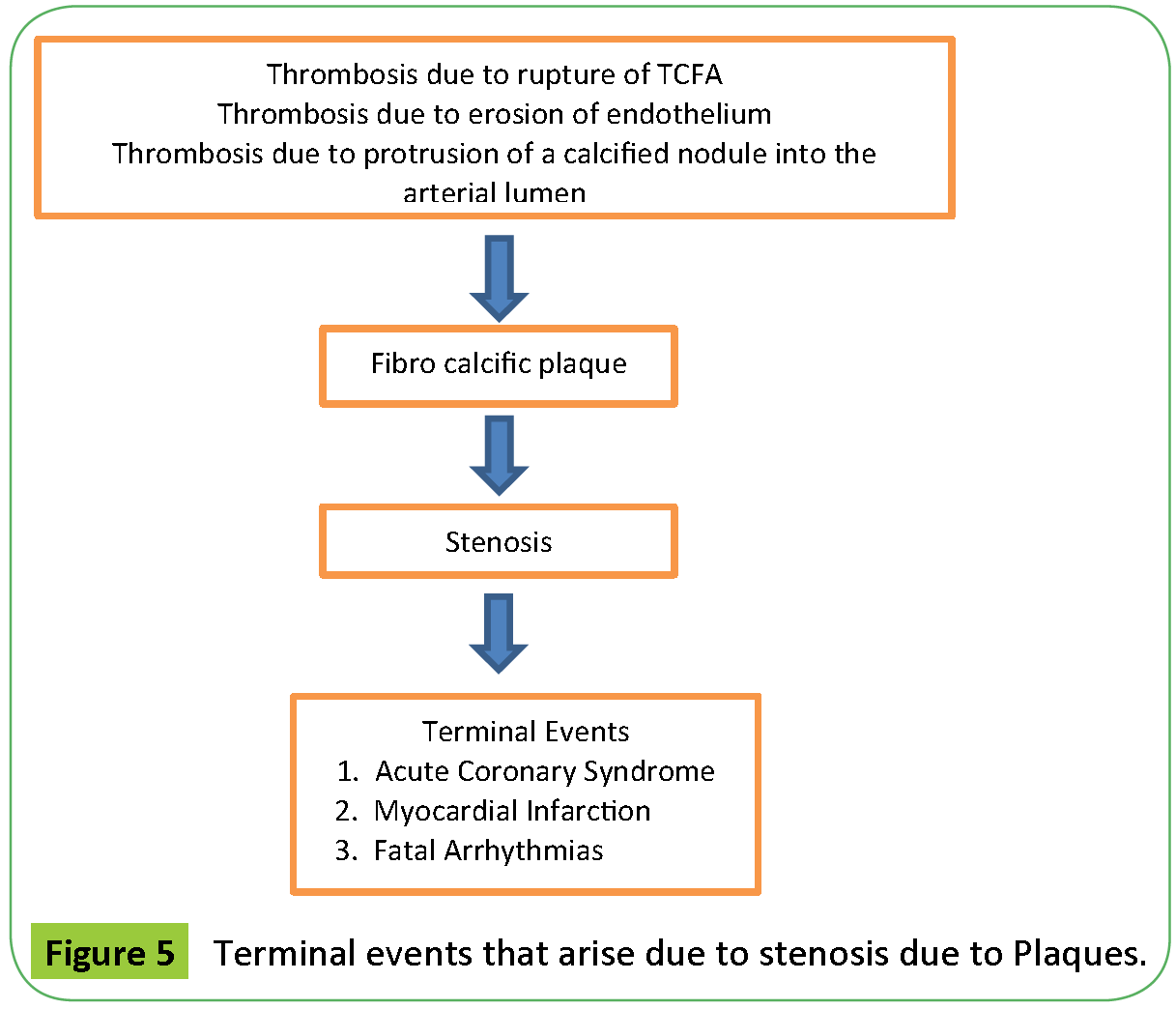
The end result of the stenosis caused by the plaques are the Terminal Events-Acute Coronary Syndrome, Myocardial Infarction, Fatal Arrhythmias, Sudden Cardiac death (Figures 4 and 5 depict the terminal events that arise due to stenosis due to plaques) [16].
Risk factors
Age, Family history, Male sex, smoking, Diabetes mellitus, hypertension, alcohol, Chlamydia infection, Hyper homocysteinemia, Obesity, Sedentary lifestyle [17].
Location
Elastic and muscular arteries. MC arteries affected are aorta, carotid, coronary and ileofemoral arteries. MC artery to be involved is Aorta. Branch points are the common sites. Proximal coronary arteries are more susceptible [18].
Clinical features
Atherosclerosis is initially asymptomatic [19]. Symptoms develop when lesions impede blood flow. When plaques grow, arterial lumen is reduced causing transient ischemic symptoms, stable exertional angina, intermittent claudication, unstable angina, infarction, ischemic stroke, rest pain in the limbs, aneurysm, arterial dissection, sudden death [20].
Diagnosis
Patients with signs and symptoms of ischemia should be evaluated using history, physical examination, fasting lipid profile, plasma glucose and HbA1c. Patients with documented disease at one site should be evaluated at other sites.
CT Angiography, is often used as an initial screening test [21]. Other diagnostic procedures used are catheter based tests-intravascular ultrasonography, angioscopy, plaque thermography, elastography, immunoscintigraphy. Certain serum inflammatory markers CRP, LP associated phospholipase A2 predict cardiovascular events. Other Imaging studies that detect plaque are–Angiography, USG, CIMT, MRI.
Treatment
Behavior Modifications include a diet rich in fruits, vegetables, fibers with regular physical activity and smoking cessation could help in getting a favourable lipid profile. Drugs to treat Dyslipidemia, hypertension and diabetes are often required. These help in improving endothelial function, reducing inflammation and give a favourable clinical outcome. Additional drugs used are statins, antiplatelet drugs (aspirin, clopidogrel), ACE inhibitors and Beta Blockers. Aspirin is indicated for prevention of coronary atherosclerosis in high risk patients. Clopidogrel is used for patients who are intolerant to aspirin and also for treating ST segment and non ST segment elevation MI. Statins, ACE inhibitors, ARB reduce risk of atherosclerosis with their anti-inflammatory properties. Statins by stabilizing the plaques, play vital role in management of atherosclerosis.
Statins induce changes in plaque tissues, hence are important in causing regression in atherosclerosis (Table 2 discusses the Statins induced changes in plaque tissues) [4,11,18].
|
1. Alter Plaque Size |
Table 2: Statins induced changes in Plaque tissues.
Fish oil supplements-Omega 3 fatty acids play vital role in creating favourable lipid profile. Vitamins–Folate, vitamin B6 and B 12 treat hyper homocysteinemia which is an important cause of Dyslipidemia.
Conclusion
Atherosclerosis is the leading cause of death in the developed countries. Deep understanding of the causes and underlying mechanism of pathogenesis will help to delineate causes and will help to plan out innovative management. As our knowledge about the pathogenesis of atherosclerosis improves more treatment options will emerge.
References
- Virmani R, Burke AP, Farb A, Kolodgie FD (2006) Pathology of the vulnerable plaque. J Am CollCardiol 47:C13-C18.
- Aschoff L (1933) Introduction. In: Cowdry EV (ed.) Arteriosclerosis: A Survey of the Problem. Macmillan, New York.
- Beaglehole R, Magnus P(2002) The search for new risk factors for coronary heart disease: occupational therapy for epidemiologists? Int J Epidemiol31: 1117-1122.
- Alexander RW, Dzau VJ (2000) Vascular biology: the past 50 years. Circulation 102: IV-112-IV-116.
- Pedrigi RM, de Silva R, Bovens SM, Mehta VV, Petretto E, et al. (2014) Thin-cap fibroatheroma rupture is associated with a fine interplay of sand wall stress. ArteriosclerThromb VascBiol34:2224-2231.
- Collins R, Armitage J, Parish S, Sleigh P, Peto (2003) R: MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo-controlled trial. Lancet 361: 2005-2016.
- Libby P (2002) Inflammation in atherosclerosis. Nature420: 868-874.
- Meijer WT, Hoes AW, Rutgers D, Bots ML, Hofman A, et al. (1998) Peripheral arterial disease in the elderly: the Rotterdam Study. ArteriosclerThrombVascBiol 18: 185-192.
- Simoons L, Saelman M (1994) Effect of simvastatin on coronary atheroma: the Multicentre Anti-Atheroma Study (MAAS). Lancet 344: 633-638.
- Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM, et al. (2009) Reduction in C-reactive protein and LDL cholesterol and cardiovascular event rates after initiation of rosuvastatin: a prospective study of the JUPITER trial. Lancet 373: 1175-1182.
- Fowkes FG, Housley E, Riemersma RA, Macintyre CC, Cawood EH, et al. (1992) Smoking, lipids, glucose intolerance, and blood pressure as risk factors for peripheral atherosclerosis compared with ischemic heart disease in the Edinburgh Artery Study. Am J Epidemiol 135: 331-340.
- Scott G, Diane B, Luther C, Richard C, Margo D, et al. (2001) Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 285: 2486-2497.
- Ingolfsson IO, Sigurdsson G, Sigvaldason H,Thorgeirsson G, Sigfusson N,et al. (1994) A marked decline in the prevalence and incidence of intermittent claudication in Icelandic men 1968-1986: a strong relationship to smoking and serum cholesterol: the Reykjavik Study. J ClinEpidemiol47: 1237-1243.
- Jonason T, Bergstrom R (1987) Cessation of smoking in patients with intermittent claudication: effects on the risk of peripheral vascular complications, myocardial infarction and mortality. Acta Med Scand221: 253-260.
- Rodriguez-Granillo GA, Agostoni P, Garcia-Garcia HM, Biondi-Zoccai GG, McFadden E (2007) Meta-analysis of the studies assessing temporal changes in coronary plaque volume using intravascular ultrasound. Am J Cardiol 99: 5-10.
- Naghavi M, Libby P, Falk E, Casscells SW, Litovsky S, et al. (2003) From vulnerable plaque to vulnerable patient a call for new definitions and risk assessment strategies: part I. Circulation108:1664-1672.
- Quick CR, Cotton LT (1982) The measured effect of stopping smoking on intermittent claudication. Br J Surg69: S24-S26.
- Silva Marques J, Pinto FJ (2014)The vulnerable plaque: Current concepts and future perspectives on coronary morphology, composition and wall stress imaging. Rev Port Cardiol33:101-110.
- Law M, Tang JL (1995)An analysis of the effectiveness of interventions intended to help people stop smoking.Arch Intern Med155: 1933-1941.
- Cannon CP, Braunwald E, McCabe CH, Rader DJ, Rouleau JL, et al. (2004)Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med 350: 1495-1504.
- Rosamond W, Flegal K, Furie K, Go A, Greenlund K, Haase N, et al. (2008) Heart disease and stroke statistics−2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 117:e25-e146.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences