Patients Diagnosed with Bipolar Mood Disorder Admitted in Private Hospitals for Covid-19 Related Diagnosis and Other Types of Diagnosis, A Restricted Scheme Case Study- South Africa
Michael Mncedisi Willie
DOI10.36648/2471-299X.21.7.124
Michael Mncedisi Willie*
Council for Medical Schemes, Policy Research and Monitoring, South Africa
- *Corresponding Author:
- Michael Mncedisi Willie
Council for Medical Schemes, Policy Research and Monitoring, South Africa
E-mail: m.willie@medicalschemes.co.za
Received Date: February 12, 2021; Accepted Date: March 18, 2021; Published Date: March 25, 2021
Citation: Willie MM (2020) Patients Diagnosed with Bipolar Mood Disorder Admitted in Private Hospitals for Covid-19 Related Diagnosis and Other Types of Diagnosis, A Restricted Scheme Case Study- South Africa. Med Clin Rev Vol.7 No.2:124
Abstract
The advent of the COVID-19 epidemic has adversely affected health systems globally. Most of the health systems are overwhelmed due to the unprecedented spread of the virus. Previous outbreaks have had persistent mental health effects, the 2003 Severe Acute Respiratory Syndrome (SARS) pandemic, significantly elevated rates of psychiatric disorders and psychological distress such as Bipolar mood disorder (BMD). The objective of this study was to assess patients of restricted schemes that have confirmed positive for COVID-19 and diagnosed with BMD. This study followed a descriptive cross-section analysis of restricted schemes claims information COVID-19. The review period was a service date between May-August 2020. Patients included were those diagnosed with BMD and had a laboratory confirmation (RT – PCR assay) hospitalisation. The analysis covered a total of 89 restricted medical scheme patients diagnosed with BMD who were admitted for suspected COVID-19 infection. The median age of patients admitted to the hospital was 48 (IQR 39-54). The median number of inpatient days was seven (IQR 4-11) and six (IQR 3-12), for the confirmed COVID-19 diagnosis and other non-COVID diagnoses, respectively. The median risk-benefit paid for the confirmed diagnosis per event was R26 704: (IQR R12 165-R46 232). The median number of inpatient days for confirmed COVID-19 diagnosis in the general ward was three (IQR 2-9), slightly lower than for those who were admitted for other reasons, with a median of 5.5 (IQR 2-11) days. There were significantly fewer patients admitted to high care and ICU in both categories. Non-COVID-19 reasons for admission included physical therapy as the second most prevalent primary admission diagnosis, while others were BMD-related diagnoses such as bipolar affective disorder, or current, mixed and severe depression, without psychotic symptoms. The study revealed evidence that patients of medical schemes are experiencing co-payments on health services that should receive PMB level of care and should be covered in full as per the regulations. Psychiatric disorders and psychological distress such as BMD are key to a multidisciplinary approach to dealing with COVID-19.
Keywords
Bipolar mood disorder (BMD); COVID-19; Medical schemes; Prescribed Minimum Benefits (PMB); Severe Acute Respiratory Syndrome (SARS)
Introduction
The COVID-19 epidemic has adversely affected socio-economic dynamics and health systems globally. The high speed of both international transmissions and the sudden increase in numbers of new diagnosis startled and rapidly overwhelmed public and private health services in South Africa (SA) [1]. Most health systems worldwide are overwhelmed because of the unprecedented spread of the virus. There are already signs of health systems collapse in some of the developed countries. Previous outbreaks have had persistent mental health effects, the 2003 Severe Acute Respiratory Syndrome (SARS) pandemic, significantly elevated rates of psychiatric disorders and psychological distress [2,3].
There is comprehensive literature that depicts the relationship between Bipolar Mood Disorder (BMD) risk factors and SARS-CoV- 2. Other studies have implicated Coronavirus infection with major depression and bipolar disorder [4,5]. Karrour and colleagues argued that risk factors for serious COVID-19 complications are also common in BMD patients [6]. According to Stefana and colleagues, treatment options for SARS-CoV-2 for patients with bipolar disorder have a likelihood of worsening mood symptoms causing instability [7]. However, Barber and colleagues found no evidence of an increased risk of contracting SARS-CoV-2 in patients with BMD [8,9]. Numerous studies have examined the effect of gender differences on patients with bipolar disorder [10-12]. The prevalence of BMD in the medical scheme has increased by more than ten in the past 9 years in medical schemes [13]. Chronic conditions such as Bipolar Mood Disorder (BMD) is Prescribed Minimum Benefits (PMB) which are a set of defined benefits to ensure that all medical scheme1members have access to certain minimum health services, regardless of the benefit option they have selected [14,15].
Objectives
The objective of this study was to assess BMD patients of a restricted scheme2 that were admitted for a COVID-19 related diagnosed.
Study Design
This study followed a descriptive cross-section analysis of restricted schemes claims information COVID-19. The review period was a service date between May-August 2020 patients included were those with laboratory confirmation (RT – PCR assay) of infection with the COVID-19. Primary ICD-10 admission diagnosis was used to identify and classify the condition into four groups. The first two groups were COVID-19 confirmed and suspected diagnosis as follows:
• A laboratory-confirmed (RT – PCR assay) COVID-19 was used to identify the COVID-19 case as per the World Health (WHO) guidelines and definition. Inclusion criteria for COVID-19 admissions were patients that had a laboratoryconfirmed (RT – PCR assay) COVID-19. The World Health Organization (WHO) defines ICD-10 codes ‘U07.1’ and ‘U07.2’ as follows [16,17]:
• An emergency ICD-10 code of ‘U07.1 COVID-19, virus identified’ is assigned to a diagnosis of COVID-19 confirmed by laboratory testing.
• An emergency ICD-10 code of ‘U07.2 COVID-19, virus not identified’ is assigned to a clinical or epidemiological diagnosis of COVID-19 where laboratory confirmation is inconclusive or not available.
• Both U07.1 and U07.2 may be used for mortality coding (cause of death).
Patients who had a hospital admissions diagnosis linked to BMD diagnosis as depicted in Table 1 below:
| F31.0 | Bipolar affective disorder, current episode hypomanic |
| F31.1 | Bipolar affective disorder, current episode manic without psychotic symptoms |
| F31.2 | Bipolar affective disorder, current episode manic with psychotic symptoms |
| F31.3 | Bipolar affective disorder, current episode mild or moderate depression |
| F31.4 | Bipolar affective disorder, current episode severe depression without psychotic symptoms |
| F31.5 | Bipolar affective disorder, current episode severe depression with psychotic symptoms |
| F31.6 | Bipolar affective disorder, current episode mixed |
| F31.7 | Bipolar affective disorder, currently in remission |
| F31.8 | Other bipolar affective disorder |
| F31.9 | Bipolar affective disorder,unspecified |
Table 1 Applicable codes for BMD [18].
Results
Demographic characteristics
The analysis covered a total of 89 restricted scheme patients diagnosed with BMD with a median age of 48 (IQR 39-54) years who were admitted to the hospital for COVID-19 related diagnosis or other types of diagnosis. The remaining 73% (n=65) were admitted for other reasons not related to COVID-19. (Table 2) depicts the different demographic characteristics of COVID- 19-confirmed diagnosis and other types of diagnosis, stratified by gender and age bands. Females made up 79% (n = 70), many study participants.
| Category | Confirmed Case | Other Case | Grand Total | Chi-Squared (P-Values) |
|---|---|---|---|---|
| Gender | ||||
| n (%) | n (%) | n (%) | ||
| Female | 20 (83) | 50 (77) | 70 (79) | 0.429 (0.513) |
| Male | 4 (17) | 15 (23) | 19 (21) | |
| Age Categories | ||||
| 15 to 24 years | 1 (4) | 3 (5) | 4 (4) | 4.497 (0.480) |
| 25 to 34 years | 2 (8) | 8 (12) | 10 (11) | |
| 35 to 44 years | 7 (29) | 15 (23) | 22 (25) | |
| 45 to 54 years | 11 (46) | 19 (29) | 30 (34) | |
| 55 to 64 years | 2 (8) | 9 (14) | 11 (12) | |
| 65+ years | 1 (4) | 11 (17) | 12 (13) | |
Table 2 Demographic characteristics [n (%)].
83% (n = 20) of all confirmed COVID-19 diagnosis were females, while 77% (n = 50) of non-COVID-19 diagnosis were females. Among COVID-19 confirmed-patients, 12% were aged 55 years or older, compared to 31% of non-COVID-19 patients.
Utilisation of services
The median number of inpatient days for confirmed COVID-19 diagnosis in general wards was three (IQR 2-9 days); slightly lower than for those admitted for other reasons, with a median of 5.5 (IQR 2-11) days (Table 3).
| Confirmed Diagnosis (n=22) | Other Diagnosis Type (n=51) | |
|---|---|---|
| Inpatient (days) | 7 (4-11) | 6 (3-12) |
| Total risk-benefit paid (Rands) | R34 438.33 (R23 000.13 - R58 448.08) |
R34 339.5 (R16 025.1 - R52 157.64) |
Table 3 Length of stays and risk benefits paid [median (interquartile range)].
Admission trends
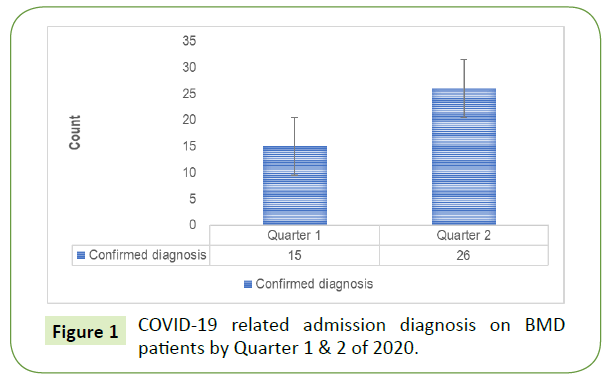
Figure 1 depicts trend data in respect of COVID-19 related admission diagnosis by quarter. The results show an increase in admissions during quarter 2. It was also evident from the data that some confirmed COVID-19 diagnosis of a patient diagnosed with BMD nearly doubled in quarter 2. The increase observed mainly in July were also consistent with the increase observed at the national level in South Africa on COVID-19 cases.
Primary admission and discharge diagnosis
Tables 4 and 5 show the top 10 admissions and discharge ICD- 10 diagnosis codes for BMD patients. Among the main reasons for primary admission, the diagnosis was confirmed diagnosis of COVID-19 (emergency use of U07.1: confirmed COVID-19 case). Table 5 shows that isolation, essential (primary) hypertension, pneumonia, unspecified dementia, unspecified HIV, unspecified dementia, delirium, unspecified and pulmonary embolism without mention of acute corpulmonale were among the most prevalent primary discharge diagnoses.
| ICD-10 Code | N | ICD-Code Description - Primary Admission Diagnosis |
|---|---|---|
| U07.1 | 30 | Emergency use of U07.1 (confirmed COVID-19 case) |
| Z50.1 | 20 | Other physical therapy |
| F31.4 | 9 | Bipolar affective disorder, current episode severe depression without psychotic symptoms |
| F32.2 | 9 | A severe depressive episode without psychotic symptoms |
| F31.6 | 6 | Bipolar affective disorder, current episode mixed |
| J22 | 6 | Unspecified acute lower respiratory infection |
| F31.9 | 5 | Bipolar affective disorder, unspecified |
| I26.9 | 5 | Pulmonary embolism without mention of acute corpulmonale |
| F31.2 | 4 | Bipolar affective disorder, current episode manic with psychotic symptoms |
| R06.0 | 4 | Dyspnoea |
Table 4 Primary admission and discharge diagnosis - Top 10: counts.
| ICD-10 Code | N | ICD-Code Description - Primary Discharge Diagnosis |
|---|---|---|
| U07.1 | 12 | Emergency use of U07.1 (confirmed COVID-19 case) |
| Z29.0 | 9 | Isolation |
| I10 | 6 | Essential (primary) hypertension |
| J18.9 | 6 | Pneumonia, unspecified |
| J22 | 6 | Unspecified acute lower respiratory infection |
| Z03.8 | 3 | Observation for other suspected diseases and conditions |
| B24 | 2 | Unspecified HIV disease |
| F03 | 2 | Unspecified dementia |
| F05.9 | 2 | Delirium, unspecified |
| I26.9 | 2 | Pulmonary embolism without mention of acute corpulmonale |
Table 5 Primary discharge diagnosis - Top 10: counts.
Logistic regression model
The outcome variable was the re-admission rate of patients diagnosed with BMD to a private hospital facility. Readmissions were defined as episodes where a patient who had been discharged from a hospital is admitted again within 30 days3 [19]. Independent variables included age, gender, admitting facility (general ward, high care and ICU) and primary diagnosis at admission (confirmed COVID-19 diagnosis vs other types of diagnosis). More than one-third of admissions were in the age band 45 to 54, followed by those in the age band 35 to 44 [34% (n=30) and 25% (n=22), respectively]. There were significant differences in the age band 45 to 54 years between patients who were re-admitted and those who were not. This was marginally significant, as depicted in Table 6. Patients in age band 15 to 24 years were associated with a decreased risk of re-admission, compared to age band 45 to 54 years (OR=0.067 CI: 0.005-0.823, p-value=0.055) while those in age band 55 to 64 years were associated with an increased risk of readmission compared to age band 45 to 54 years (OR=2.846 CI: 0.273-29.641, p-value=0.05).
| Effect | OR | 95% LCL | 95% UCL | P | |
|---|---|---|---|---|---|
| Gender | Female (ref) | 1 | |||
| Male | 0.879 | 0.220 | 3.509 | 0.855 | |
| 15 to 24 years | 0.067 | 0.005 | 0.823 | 0.055 | |
| 25 to 34 years | 0.209 | 0.041 | 1.054 | 0.197 | |
| Age category | 35 to 44 years | 0.223 | 0.059 | 0.846 | 0.134 |
| 45 – 54 years (ref) | 1 | ||||
| 55 to 64 years | 2.846 | 0.273 | 29.641 | 0.050 | |
| 65+ years | 1.75 | 0.183 | 16.706 | 0.136 | |
| Primary admission diagnosis | COVID-19 (ref) Confirmed case |
1 | |||
| Other case | 0.398 | 0.103 | 1.544 | 0.183 | |
| General ward (ref) | 1 | ||||
| High care | 0.104 | 0.01 | 1.054 | 0.056 | |
| Admission type facility | ICU | 0.456 | 0.03 | 6.913 | 0.995 |
| Other | 0.931 | 0.264 | 3.281 | 0.261 | |
Table 6 Logistic regression: Outcome variable readmission.
Discussion
This study sought to assess the characteristics of BMD patients admitted to private hospitals for a COVID-19-related diagnosis and other types of diagnosis. The study found that 23% of admissions among BMD patients were for COVID-19-related diagnoses. The study also revealed a rise in the number of COVID- 19-related admissions during quarter 2 of 2020, July 2020. This was consistent with the rise in COVID-19 infections nationally in South Africa. Age and gender are demographic characteristics that have been studied extensively in the literature on BMD patients. The condition is more prevalent in females than in males [20,12]. Furthermore, demographic characteristics such as age and gender have been found to increase the risk of COVID-19, mainly in older patients. The study found that the median age of patients with BMD admitted to hospitals was 48 years. A study by Jin and colleagues revealed that older age and a higher number of comorbidities were associated with greater severity and mortality in patients with both COVID-19 and SARS [21]. There were proportionately older patients diagnosed with COVID-19 than other conditions in this study.
The distribution of patients by gender is consistent with the literature. According to Mengand colleagues gender is an important biological variable that should be considered in the prevention and treatment of COVID-19 [22]. Significantly more female patients diagnosed with BMD were admitted to the hospital than males. Other studies have, however, shown that men with COVID-19 are more at risk for worse outcomes and death [21]. The median lengths of stay in the hospital for COVID- 19-related admissions and other types of admissions were similar at just under eight days, as were the median costs per event. The study found that some BMD patients were subjected to co-payments as in some instances the medical scheme did not cover the whole amount claimed. This was slightly significantly lower in COVID-19-related admissions. COVID-19 has been approved as a PMB [15]. Similarly, BMD is also a PMB condition. It is therefore worrying that some members were subjected to co-payments as high as 7% of the amount claimed.
Significantly, more COVID-19-related admissions were to the general ward, compared to other types of admissions. Few COVID-19 patients were admitted to ICU. However, several non-COVID-19 patients were admitted to ICU. This could also be attributed to increased severity in BMD patients, who had other comorbidities such as pneumonia and hypertension. The study found that demographic characteristics such as age were a risk factor for re-admission in patients with BMD, whether they were re-admitted for COVID-19 or non-COVID-19 conditions. The odds of readmission were highest among 55-64-year-olds; however, this was marginally significant. Gender was found not to be a determining factor for re-admissions. A study by Fuller and colleagues found that older age (predisposing factors) and the possession of health insurance (enabling factors) were linked to high hospitalisation rates [23].
In addition to a COVID-19 BMD-related primary diagnosis, the study found that dyspnoea was one of the symptoms of admission. Dyspnoea, also known as shortness of breath or breathlessness, is a subjective awareness of the sensation of uncomfortable breathing. The other main reasons were pneumonia, meningitis, essential tremor bronchopneumonia, unspecified acute renal failure, and unspecified chest pain. A study by Leitmeyerand colleagues showed that a dry cough, chest pain and dyspnoea were prominent in patients with lower respiratory tract symptoms on admission [24]. The study found that BMD patients admitted to hospital were susceptible to other chronic conditions such as essential (primary) hypertension, pneumonia and unspecified HIV disease. This gives insights into other chronic conditions that may be prevalent in patients diagnosed with BMD.
Conclusion
The study revealed evidence that patients diagnosed with BMD are also at high risk of being admitted to a hospital for COVID-19 related diagnosis. The majority of these are admitted were in an outpatient setting. It is concerning that some patients were subjected to co-payments for treatment of PMB conditions such as BMD and COVID-19, even though both these conditions are PMB level care where medical schemes need to cover in full [25,15]. Isolation was found to be one of the most prevalent discharge diagnoses, thus indicating a further challenge for patients diagnosed with BMD who need continued care and observation. The social environment is important for keeping mentally ill persons functioning well in the community and for reducing the likelihood of recurrence of mental illness symptoms [26,27]. Thus, indicating possible challenges that BMD patients face in as far self-isolation and other much needed support from family members. This becomes even more important during unprecedented times like the COVID-19 pandemic. Psychiatric disorders and psychological distress such as BMD are key to a multidisciplinary approach to dealing with COVID-19. It is concerning that some patients were subjected to co-payments for treatment of PMB conditions such as BMD and COVID-19. Further work is much needed to assess the schemes and administrator system capabilities in the identification of PMB level of care conditions relative to co-payments which further adds financial burden to members.
Limitations and Future Research
The study did not conduct a comprehensive analysis of condition-specific readmissions, furthermore, the study did not consider severity and patients with comorbidities that were admitted in hospitals [28], these key attributes could certainly enhance the findings of this study. An industry-wide similar study could certainly provide better insight at the industry level could assist policymakers to make an informed decision on key interventions on COVID-19. Future research should entail detailed analysis and audit of discharge diagnosis, including those that are related to mortality [29-31].
Competing Interests
None
1A medical scheme helps you to pay for your healthcare needs, such as nursing, surgery, dental work, medicine and hospital accommodation. You pay monthly contributions in order to have medical cover.
2Restricted or closed medical schemes are typically much smaller in membership numbers than open schemes.
3https://en.wikipedia.org/wiki/Hospital_readmission
References
- Wu Z, McGoogan JM (2020) Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 diagnoses from the Chinese Center for Disease Control and Prevention. JAMA 323(13): 1239-1242.
- Wu P, Fang Y, Guan Z. (2009)The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry 54: 302-311.
- Tabata S, Imai K, Kawano S (2020) Clinical characteristics of COVID-19 in 104 people with SARS-CoV-2 infection on the Diamond Princess cruise ship: A retrospective analysis. Lancet Infect Dis 20: 1043-1050.
- Severance EG, Dickerson FB, Viscidi RP(2011) Coronavirus immunoreactivity in individuals with a recent onset of psychotic symptoms. Schizophr Bull 37(1): 101-107.
- Okusaga O, Yolken RH, Langenberg P (2011) Association of seropositivity for influenza and coronaviruses with history of mood disorders and suicide attempts. J Affect Disord 130: 220-225.
- Karrouri R, Hammani Z, Otheman Y (2020) Managing bipolar disorder in time of COVID-19 pandemic. J Med Clin Res 1: 20-23.
- Stefana A, Youngstrom EA, Chen J (2020) The COVID-19 pandemic is a crisis and opportunity for bipolar disorder. Bipolar Disord.
- Barber S, Thornicroft G (2018) Reducing the mortality gap in people with severe mental disorders: the role of lifestyle psychosocial interventions. Front Psychiatry 9:463.
- Kim, Andrew Wooyoung. “Evaluating the Mental Health Impacts of the COVID-19 Pandemic in Urban South Africa: Perceived Risk of COVID-19 Infection and Childhood Trauma Predict Adult Depressive Symptoms.” medRxiv: the preprint server for health sciences 2020.06.13.20130120.
- Hendrick V, Altshuler LL, Gitlin MJ, Delrahim S, Hammen C (2000) Gender and bipolar illness. J Clin Psychiatry 61: 393-396.
- Frye MA, Altshuler LL, McElroy SL (2003) Gender differences in prevalence, risk, and clinical correlates of alcoholism comorbidity in bipolar disorder. Am J Psychiatry 160(5): 883-889.
- Vega P, Barbeito S, de Azua SR (2011) Bipolar disorder differences between genders: special considerations for women. Women’s Health (LondEngl) 7: 663-674.
- Willie MM (2020) The Utilisation of Psychiatry and Other Mental Health Benefits by Members of Medical Schemes, South Africa. Med Clin Rev 6(5): 106
- Council for Medical Schemes (CMS) (2019) Draft PMB definition guidelines for bipolar mood disorder. Council for Medical Schemes. Pretoria. South Africa.
- Council for Medical Schemes (CMS) (2020) PMB definition guideline: COVID-19 v2 05 May 2020. Pretoria: CMS.
- World Health Organization (2020) Media Statement: Knowing the Risks for COVID-19.
- World Health Organization(2020) Emergency use ICD codes for COVID-19 disease outbreak. Geneva: WHO.
- Council for Medical Schemes (CMS)(2018) Circular 59 of 2018. Mental Health Conditions. Council for Medical Schemes. Pretoria. South Africa.
- Himmels JPW, Borge TC, Brurberg KG, Gravningen KM, Feruglio SL, et al. (2020) COVID-19: COVID-19 and risk factors for hospital admission, severe disease, and death: Norwegian Institute of Public Health.
- Naguy A (2017) Bipolar in women: any gender-based difference? Indian J Psychol Med 39: 381-382.
- Jin JM, Bai P, He W (2020) Gender differences in patients with COVID-19: Focus on severity and mortality. MedRxiv.
- Meng Y, Wu P, Lu W (2020) Sex-specific clinical characteristics and prognosis of coronavirus disease-19 infection in Wuhan, China: a retrospective study of 168 severe patients PLoS Pathog 16: 1-13.
- Fuller RL, Atkinson G, McCullough EC, Hughes JS (2013) Hospital readmission rates: the impacts of age, payer, and mental health diagnoses. J Ambulatory Care Manage 36(2): 147-55.
- Vu HT, Leitmeyer KC, Le DH (2004) The clinical description of a completed outbreak of SARS in Vietnam, February-May 2003. Emerging Infectious Diseases 10(2): 334-338.
- Council for Medical Schemes (CMS)(2010) Code of Conduct in respect of PMB benefits. Council for Medical Schemes. Pretoria. South Africa.
- Iseselo MK, Kajula L, Yahya-Malima KI (2016) The psychosocial problems of families caring for relatives with mental illnesses and their coping strategies: a qualitative urban-based study in Dar es Salaam, Tanzania. BMC Psychiatry 16: 146.
- Van Rheenen TE, Meyer D, Neill E (2020) Mental health status of individuals with a mood disorder during the COVID-19 pandemic in Australia: Initial results from the COLLATE project. J Affect Disord 275: 69-77.
- Yang J, Zheng Y, Gou X (2020) Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: A systematic review and meta-analysis. Int J Infect Dis 94: 91-95.
- Donnelly J, Qing Wang X, Iwashyna T (2020) Readmission and Death After Initial Hospital Discharge Among Patients With COVID-19 in a Large Multihospital System. JAMA e2021465.
- Biagi L, Rossi A, Malagoli A (2020) Clinical and epidemiological characteristics of 320 deceased Covid-19 patients in an Italian province: a retrospective observational study. J Med Virol 92(11):2718-2724.
- Kuehn BM (2020) Hospital Readmission Is Common Among COVID-19 Survivors. JAMA 324(24): 2477.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences