Pulmonary Rehabilitation for Patients with COVID-19
Meena Gupta* and Divya Pandey
Divya Pandey and Meena Gupta*
Amity Institute of Physiotherapy, Amity university, Noida, Uttar Pradesh, India
- *Corresponding Author:
- Meena Gupta
Amity Institute of Physiotherapy, Amity university, Noida, Uttar Pradesh, India
E-mail: aikabir@yahoo.com
Received Date: May 28, 2021; Accepted Date: June 14, 2021; Published Date: June 21, 2021
Citation: Pandey D, Gupta M (2021) Pulmonary Rehabilitation for Patients with COVID-19. Med Clin Rev Vol.7 No.6:139.
Abstract
COVID-19 also referred to as coronavirus disease 2019 is an infectious contamination disease, which may cause respiratory, physical, mental, and local systemic failure. The seriousness of this disease ranges from an asymptomatic disease or gentle ailment to mellow or extreme pneumonia with respiratory collapse as well as death. The aim of pulmonary rehabilitation in COVID-19 patients is to improve manifestations of dyspnea, relieve uneasiness, diminish complications, limit disability, protect function and improve quality of life. Pulmonary rehabilitation during the acute management of COVID-19 ought to be viewed as whenever the situation allows and safe and may incorporate proper nutrition, posture, airway, oxygen supplementation, clearance technique, postural drainage, breathing exercises, stretching, active range of motion (ROM) exercises, manual therapy and physical activities. Given the chance of long term disability, outpatient post-hospitalization pulmonary rehabilitation might be considered in all patients hospitalized with COVID-19. This review serves as a guide and launching point for the ongoing management of functional and comorbid rehabilitative issues related to COVID-19.
Keywords
COVID-19, Pulmonary Rehabilitation, Quality of Life
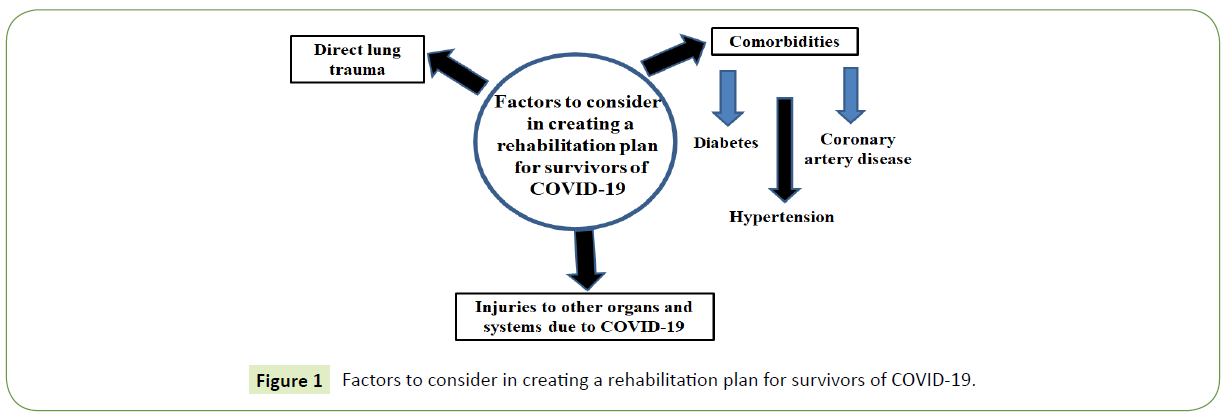
COVID-19 also described as novel Coronavirus infection 2019 by the World Health Organization (WHO), COVID-19 is a respiratory tract contamination brought about by SARS-CoV-2, a coronavirus. Coronavirus first showed up in Wuhan region of China in the late December 2019 The first case in Turkey was distinguished on March eleventh, 2020. The WHO proclaimed COVID-19 as a pandemic on March twelfth, 2020. The aim of pulmonary rehabilitation in COVID-19 patients is to improve manifestations of dyspnea, mitigate anxiety, decrease complications, limit disability, safeguard function and improve quality of life [1]. Pulmonary recovery ought to be custom fitted to every individual patient. Pulmonary rehabilitation’s definition, as adapted from the American Thoracic Society/European Respiratory Society, is comprehensive intervention dependent on a careful patient evaluation followed by understanding custom fitted treatments that incorporate, however are not restricted to, exercise training, education, and conduct change, intended to improve the physical conditions of individuals with respiratory ailment [2]. Coronavirus patients will frequently give prior comorbidities and this must be thought about in the restoration plan for the patient (Figure 1).
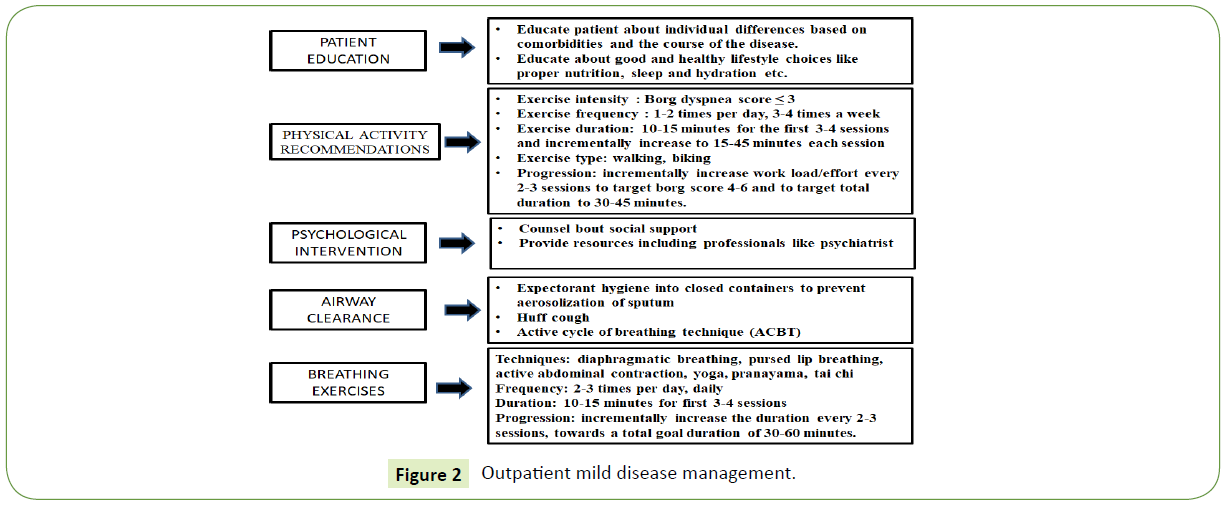
Outpatient mild disease management
Mild disease is characterized as gentle side effects without pneumonia appearances on imaging [3]. Rehabilitation for gentle illness can be overseen in the outpatient setting utilizing telemedicine [4]. In mellow sickness, pulmonary recovery might be thought of and incorporate training, airway clearance techniques, physical exercise, breathing activities, and anxiety management. Refer to the image below for details (Figure 2).
Specifically, sufficient dealing with and removal of corporal liquid ought to be practiced in home establish pulmonary recovery units. Patients ought to be told to cover nose and mouth with tissue when coughing or sneezing with the quick disposal of the tissue. Expectorant hygiene into a closed holder ought to be reinforced to forestall aerosolization of sputum. Hand cleanliness with hand washing subsequent to having contact with respiratory emissions and contaminated items/materials ought to be stressed. Patients should be instructed on the clinical course of COVID-19 and with individualization dependent on persistent comorbidities of the patient [5]. The patient, including asymptomatic relatives, might be directed to wear masks; (2) Sars-CoV2 has a high transmission rate and a long asymptomatic prodromal stage with a scope of 2-14 days and a mean of 3-7 days [6]. Mathematical demonstrating shows that using mask with 50% compliance during a viral flare-up can control the spread with a 50% lessening in pervasiveness and 20% abatement in aggregate frequency.
Breathing activities might be utilized at this stage. Diaphragmatic breathing includes training the patient to dominatingly engaging the diaphragm while limiting the activity of extra muscles [7]. Nasal inspiration ought to be urged to encourage in order to facilitate recruitment of diaphragm and enhance humidification [8]. Active abdominal muscle contraction ought to be utilized toward the end of expiration to increase the abdominal pressure and push the diaphragm up to a more good length-tension [9]. Yoga and specifically Viniyoga arranges breathing with arm lifts or body situating during the inspiratory or expiratory stage. Pranayama, Tai Chi [10], and singing additionally utilize coordinated breathing methods.
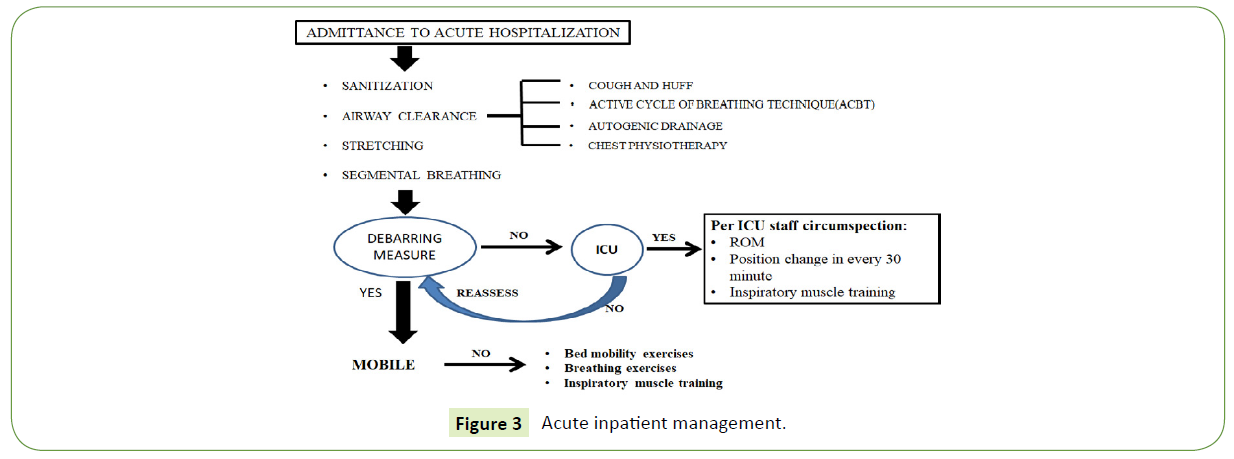
Acute inpatient management
Moderate to extreme malady is characterized as indicative patients with or moving toward respiratory distress with respiratory rate> 30 times/minutes, oxygen saturation at rest <93%, or PaO2/FiO2<300 mmHg. These individuals require hospitalization and continuous monitoring.
Pneumonic recovery during intense administration of COVID-19 ought to be viewed as whenever the situation allows and is summed up in Figure 3 given below. In acute aggravation of chronic lung conditions, pulmonary rehabilitation brings about moderate to huge impacts on wellbeing related personal satisfaction and exercise capacity [11]. Overall, pulmonary recovery in acute disease gives off an impression of being protected with no expanded mortality [12] and can be safely executed for COVID-19 [13].
Rehabilitation interventions during acute hospitalization
Early pulmonary rehabilitation and mobilization in the ICU might be approached with mindful thought and ought not to happen to the detriment of medical care worker safety [14]. SARS-CoV2 aerosolizes during methods and in ICU environments [15]. To save individual protective equipment and given the flawed result of early assembly in the ICU, early preparation by extra recovery staff isn't suggested in the ICU and might be a thought by committed ICU staff. Respiratory muscle weakness from diaphragm proteolysis may happen after delayed mechanical ventilation 18 and inspiratory muscle training may happen during weaning preliminaries with a skilled respiratory therapist [16,17]. Inception of pulmonary restoration in the inpatient setting ought to happen in light of wellbeing rules. Around 3% to 5% of in any case healthy patients can advance inside 7 to 14 days of disease to extreme or even critical conditions. Therefore, initial intensity of any physical activity ought to be reviewed and drawn nearer with alert and observing. Rejection measures incorporate the accompanying:
1. Temperature of the body > 38.0°C;
2. Introductory diagnosis time or manifestation beginning ≤ 3 days;
3. Initial beginning of dyspnea ≤ 3 days;
4. Chest picture progression inside 24 to 48 hours > 50%;
5. SpO2 ≤ 90%;
6. Blood pressure <90/60 mmHg or > 180/90 mmHg;
7. Respiratory rate > 40 times/min;
8. Pulse <40 beats/min or > 120 beat/min;
9. New beginning of arrhythmia and myocardial ischemia;
10. Level of consciousness altered.
Physical exercise is a core part of pulmonary recovery and may begin with bed mobility in the much deconditioned patient to strolling in the mobile patient. Rehabilitation mediation should target SpO2 > 90% with titration of supplemental oxygen to keep up target saturation. Pause in action ought to happen if SpO2 dips under objective or Borg scale dyspnea score > 3 with thought of breathing strategy like pursed lip breathing with resumption of activity intercession once SpO2 comes to target [18]. Pursed lips breathing is performed via nasal inspiration followed by expiratory blowing against pursed lips to diminish airway breakdown, decrease respiratory rate and dynamic hyperinflation during exercise with the point of a general increment in the endurance [19]. Oxygen supplementation has additionally been effectively utilized during exercise training to help unload the muscles of respiration. Pulmonary rehabilitation or breathing activities ought to be halted if SpO2 doesn't recoup and the patient can't keep up Borg scale dyspnea score <4, with rest and oxygen supplementation. Recovery activities ought to likewise stop for chest pain, palpations, and dizziness. The Borg Scale is an approved and simple to utilize apparatus for patients to self-screen respiratory exertion with a nearby connection between the greatness of respiratory exertion and the power of dyspnea [20].
ACBT uses cycles and combination of airway clearance procedures to ventilate clogged lung segments [21]. No particular strategy has discovered to be better than over others and should be construct on training and expertise [22]. Autogenic drainage is a typical method that uses a blend of the maneuver’s to activate and bring together discharges with short breaths to gather emissions in peripheral airway, trailed by ordinary breaths to gather discharges into the intermediate airway, and full deep breaths and huff cough to expel the secretions out [23].
Use of airway clearance techniques (ACT) can essentially lessen the requirement for ventilatory help, long periods of mechanical ventilation and hospitalization. ACT intend to help airway clearance by moving bodily fluid in a cephalic bearing from the peripheral to upper airway route, advancing the enlistment of lung volume, and wiping out bodily fluid by cough or forced expectoration.6 Physical exercise is a foundation of pulmonary rehabilitation and has been appeared to encourage airway clearance. In acute stages, early mobilization and physical exercise are liked and more compelling than bodily fluid clearance procedures and mucus removing/clearing techniques ought not to be utilized alone or overshadow physical movement.
Lung volume enlistment maneuvers incorporate air stacking and glottis holding. Air stacking includes conveyance of air through Ambu bag [24]. Glossopharyngeal breathing is a type of positive pressure breathing strategy that can be utilized to help failing respiratory muscles and increases tidal volume. It includes progressive breathe in of boluses of air and driving them into the lungs [25]. The 3-second breath hold is a technique for ventilating obstructed lung portions. A pause for 3 seconds takes into account Pendelluft stream where air moves from unhindered districts to the deterred locales of the lung [26].
Constrained expiration maneuvers like the huff cough can be utilized to impel secretions. huff cough is performed with an open glottis where equivalent pressure point dynamic compression of the airway routes makes an expansion in the linear speed of the expiratory airflow and drives emissions. Starting a constrained expiration at a low lung volume moves the equivalent pressure points to the periphery and the small airways. A constrained expiration from a high lung volume will move the equivalent pressure point halfway towards the enormous focal airway [27]. Body posture assumes a significant part in respiratory function and patients can be urged to participate in erect head and neck positioning during respiratory treatment and consistently whenever the situation allows. External vibration if accessible might be applied with oscillation frequencies under 17 Hz to improve mucociliary clearance. Positioning is efficacious, easy, and simple to accomplish [28]. Positioning might be ideal over different strategies like postural drainage given the pathophysiology of COVID-19 and the observed V/Q mismatch [29,30]. Sitting and standing are the favored situations in non-critically sick patients to amplify lung work including FVC, increase lung compliance and elastic recoil, and shift mediastinal structures, and supply mechanical advantage in constrained expiration [31]. Directed positioning might be utilized to improve ventilation, perfusion, oxygenation and mobilization of emissions in explicit lung areas of combinations through gravity. Perfusion is more prominent to the dependent lung portions in all positions [32]. Preferential ventilation changes dependent on position. Two minutes in each position while taking part in breathing activities might be adequate to ventilate/perfuse focused on lung segments. Recounted proof in clinics proposing prone positioning during acute care of COVID-19 patient has been helpful. On the off chance that conceivable, we suggest time in all positions including side-lying, upright, supine, and prone and guided by imaging discoveries whenever the situation allows. Directed positions might be dictated by the area of consolidations seen on imaging or found on examination. In the upright position, ventilation specially happens in the mid and lower lobes with perfusion most noteworthy in the lower lobes [33]. Patients may rest in a recumbent position sometimes to help in DLCO. DLCO increases in the recumbent situation in healthy subjects [34]. Supine position additionally specially ventilates the upper lobes. In an adult individual side-lying position specially ventilates the dependent lung by amplifying the length-strain proportion in the dependent hemi-diaphragm and negative pleural pressure [35]. In small kids <12-years-old side-lying position specially ventilates the nondependent lung and shutting of airway in depended areas. Side-lying might be a decent position during administration of inhaled drug with improved deposition by 13% to the reliant upper lobe. Prone positioning for two minutes span may help in ventilation to dorsal lung through decrease in lung pressure by the heart in the semi-prone situation because of ventral displacement of the heart with increments in end-expiratory trans-pulmonary pressure as well as expiratory reserve volume, more homogenous lung swelling from dorsal to ventral and improvement in oxygenation. Prone positioning has been utilized in the ICU to improve gas trade in ARDS and improve Pa/FiO2 in patients on mechanical ventilation and lessens cardiovascular comorbidities [36].
Patients might be urged to participate in routine stretching 3 times each day. Extending has been appeared to expand compliance by as much as 50mL. Stretches ought to incorporate neck, upper chest, pectoralis major, horizontal chest stretches [37] and flexion and extension to activate the facet joints. The dorsal chest wall has been demonstrated to be less compliant in patients with ARDS [38].
Osteopathic manipulations, if suitable, might be useful and should address autonomics, lymph drainage, and rib cage mobility. The patient may likewise participate in modified segmental breathing where the patient applies strain to their own thoracic cage to oppose respiratory expedition. in one region of the thoracic cavity and to encourage the expansion of nearby regions of the thoracic cavity that may have diminished ventilation and mobility [39]. Training in regards to legitimate nourishment is especially significant in COVID-19 as studies from Western nations are demonstrating that weight to be a huge danger factor for seriousness of malady with at any rate ⅔ of ICU patients having overweight BMI [40]. In obesity lung functioning is likewise impaired [41]. Similar techniques might be applied to patients recuperating from ICU level consideration. In these patients, an attention on breathing exercises and bed mobility might be the underlying intercession given the deconditioning that happens in ICU. Bed mobility exercises incorporate lower leg ankle-toe pumps, sliding legs into flexion/extension, over-head arm extends, sit-to-stand at bedside. Also, respiratory muscle shortcoming from diaphragm proteolysis might be suspected in those patients with delayed mechanical ventilation. Inspiratory and expiratory muscle training can be utilized in these patients beginning with incentive spirometry and advancing to inspiratory muscle training gadgets if accessible.
Post-Acute Rehabilitation
Propriety for inpatient acute recovery ought to be individualized to the patient [42]. Outpatient post-hospitalization pulmonary rehabilitation might be considered in all patients hospitalized with COVID-19 [43]. Patient choice criteria should be created in the coming months after the pandemic. Quadriceps weakness and altered exercise capacity might be indicators of acceptable possibility for pulmonary rehabilitation [44]. Occupational and physical therapy treatment may likewise be considered in those with functional deficits related with delayed hospitalization.
Routine observing with chest x-ray and PFT might be considered in the outpatient setting especially inside a half year of contamination and for extreme and critical patients. pulmonary fibrosis may happen in COVID-19. In SARS-CoV in 2003, pulmonary fibrosis apparently developed in 45% of patients (analyzed by X-ray and CT scan) multi month after contamination, 30-36% 3-6 months after infection [45], and 28% 1 year after infection. After SARS-CoV disease, seriousness of fibrosis and handicap corresponded with the seriousness and span of illness [46,47]. Improvement in lung functioning in SARS-CoV patients leveled at a half year with continued disability especially in DLCO 2 years after infection [48].
Pulmonary rehabilitation in the post-acute period may progress in the direction of progress in exercise capacity of the individual. In patients with interstitial lung malady, exertional desaturation is a key component and is regularly more extreme than that seen in other pulmonary conditions [49]. Interstitial lung ailment is related with diminished ventilatory limit and tissue oxygenation with untimely beginning of metabolic acidosis with dyspnea and lower limb distress/weakness during sub-maximal exercise [50]. Pulmonary hypertension likewise be present and decline exercise capacity [51]. Supplemental oxygen might be expected to encourage oxygenation of tissue and upgrade exercise limit with target SpO2 from 85 to 90%.
Conclusion
Rehabilitation may assume a significant part in reestablishing capacity and restricting disability this pandemic. Pulmonary Rehabilitation give us extra devices in the battle against COVID-19 and may incorporate nourishment, airway, posture, clearance techniques, oxygen supplementation, breathing activities, stretching, manual treatment, and physical activity. In the months to years following this pandemic, the weight of sickness might be huge and the physiotherapist may assume a crucial function in the restoration of patients with disability in relation to COVID-19.
References
- Chinese Association of Rehabilitation Medicine (2020) Respiratory rehabilitation committee of Chinese Association of Rehabilitation Medicine, Cardiopulmonary rehabilitation Group of Chinese Society of Physicai Medicine and Rehabilitation.
- Spruit MA, Singh SJ, Garvey C (2013) An Official American Thoracic Society/European Respiratory Society Statement: Key Concepts and Advances in Pulmonary Rehabilitation. Am J Respir Crit Care Med 188: e13–e64.
- Lin L, Li TS (2020) Interpretation of “Guidelines for the Diagnosis and Treatment of Novel Coronavirus (2019-nCoV) Infection by the National Health Commission (Trial Version 5)”.
- Lim PA, Ng YS, Tay BK (2004) Impact of a viral respiratory epidemic on the practice of medicine and rehabilitation: severe acute respiratory syndrome. Arch Phys Med Rehabil 85:1365–1370.
- Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E (2020) Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis.
- Guo YR, Cao QD, Hong ZS (2020) The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak – an update on the status. Military Med Res 7:11.
- Gosselink R (2004) Breathing techniques in patients with chronic obstructive pulmonary disease (COPD). Chron Respir Dis 1: 163–172.
- Elad D, Wolf M, Keck T (2008) Air-conditioning in the human nasal cavity. Respir Physiol Neurobiol 163(1-3): 121–127.
- Casciari RJ, Fairshter RD, Harrison A, Morrison JT, Blackburn C, Wilson AF (1981) Effects of breathing retraining in patients with chronic obstructive pulmonary disease. Chest 79: 393–398.
- Ngai SPC, Jones AYM, Tam WWS (2016) Tai Chi for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev (6).
- Jones SE, Barker RE, Nolan CM, Patel S, Maddocks M et al., (2018) Pulmonary rehabilitation in patients with an acute exacerbation of chronic obstructive pulmonary disease. J Thorac Dis 10(S12): S1390–S1399.
- Puhan MA, Gimeno-Santos E, Cates CJ, Troosters T (2016) Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Airways Group, ed. Cochrane Database of Systematic Reviews.
- Yang F, Liu N, Hu JY, et al. (2020) Pulmonary rehabilitation guidelines in the principle of 4S for patients infected with 2019 novel coronavirus (2019-nCoV) 43: 180–182.
- Liu W, Mu X, Wang X, Zhang P, Zhao L et al. (2018) Effects of comprehensive pulmonary rehabilitation therapy on pulmonary functions and blood gas indexes of patients with severe pneumonia. Exp Ther Med.
- Wax RS, Christian MD (2020) Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth.
- Bissett B, Gosselink R, van Haren FMP (2020) Respiratory Muscle Rehabilitation in Patients with Prolonged Mechanical Ventilation: A Targeted Approach. Crit Care 24: 103.
- Paiva DN, Assmann LB, Bordin DF (2015) Inspiratory muscle training with threshold or incentive spirometry: Which is the most effective? Revista Portuguesa de Pneumologia 21: 76–81.
- Mayer AF, Karloh M, Dos Santos K, de Araujo CLP, Gulart AA (2018) Effects of acute use of pursed-lips breathing during exercise in patients with COPD: a systematic review and meta-analysis. Physiotherapy 104: 9–17.
- Kurabayashi H, Kubota K, Machida I, Tamura K, Take H (1997) Effective physical therapy for chronic obstructive pulmonary disease: Pilot Study of Exercise in Hot Spring Water1. American journal of physical medicine & rehabilitation 76(3): 204–207.
- Cullen DL, Rodak B (2002) Clinical utility of measures of breathlessness. Respir Care 47: 986–993.
- McKoy NA, Saldanha IJ, Odelola OA, Robinson KA (2012) Active cycle of breathing technique for cystic fibrosis. Cochrane Database Syst Rev 12.
- Wilson LM, Morrison L, Robinson KA (2019) Airway clearance techniques for cystic fibrosis: an overview of Cochrane systematic reviews. Cochrane Database Syst Rev 1.
- McCormack P, Burnham P, Southern KW (2017) Autogenic drainage for airway clearance in cystic fibrosis. Cochrane Database Syst Rev 10.
- Kang SW, Bach JR (2000) Maximum insufflation capacity: vital capacity and cough flows in neuromuscular disease. Am J Phys Med Rehabil 79: 222–227.
- Maltais F (2011) Glossopharyngeal breathing. Am J Respir Crit Care Med 184: 381.
- Crawford AB, Cotton DJ, Paiva M, Engel LA (1989) Effect of airway closure on ventilation distribution. J Appl Physiol 66: 2511–2515.
- McIlwaine M, Bradley J, Elborn JS, Moran F (2017) Personalising airway clearance in chronic lung disease. Eur Respir Rev 26: 160086.
- Fink JB (2002) Positioning versus postural drainage. Respir Care 47: 769–777.
- Tang X, Du R, Wang R (2020) Comparison of Hospitalized Patients with Acute Respiratory Distress Syndrome Caused by COVID-19 and H1N1.
- Gattinoni L, Coppola S, Cressoni M, Busana M, Chiumello D (2020) Covid-19 Does Not Lead to a “Typical” Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med.
- Manning F, Dean E, Ross J, Abboud RT (1999) Effects of side lying on lung function in older individuals. Phys Ther 79: 456–466.
- Dentice RL, Elkins MR, Dwyer GM, Bye PTP (2018) The use of an alternate side lying positioning strategy during inhalation therapy does not prolong nebulisation time in adults with Cystic Fibrosis: a randomised crossover trial. BMC Pulm Med 18: 3.
- Bailey DL, Farrow CE, Lau EM (2019) V/Q SPECT-Normal Values for Lobar Function and Comparison With CT Volumes. Semin Nucl Med 49: 58–61.
- Katz S, Arish N, Rokach A, Zaltzman Y, Marcus E-L (2018) The effect of body position on pulmonary function: a systematic review. BMC Pulm Med 18: 159.
- Bhuyan U, Peters AM, Gordon I, Davies H, Helms P (1989) Effects of posture on the distribution of pulmonary ventilation and perfusion in children and adults. Thorax 44: 480–484.
- Guérin C, Reignier J, Richard JC (2013) Prone Positioning in Severe Acute Respiratory Distress Syndrome. N Engl J Med 368: 2159–2168.
- Rattes C, Campos SL, Morais C (2018) Respiratory muscles stretching acutely increases expansion in hemiparetic chest wall. Respiratory Physiology & Neurobiology 254: 16–22.
- Pelosi P, D’Andrea L, Vitale G, Pesenti A, Gattinoni L (1994) Vertical gradient of regional lung inflation in adult respiratory distress syndrome. Am J Respir Crit Care Med 149: 8–13.
- Harmony WN (1956) Segmental breathing. Phys Ther Rev 36: 106–107.
- Intensive Care National Audit & Research Centre (2020) ICNARC Report on COVID-19 in Critical Care. Intensive Care National Audit & Research Centre.
- Chlif M, Temfemo A, Keochkerian D, Choquet D, Chaouachi A et al., (2015) Advanced Mechanical Ventilatory Constraints During Incremental Exercise in Class III Obese Male Subjects. Respir Care 60: 549–560.
- AAPM&R Board of Governors AAPM&R Position Statement on the Necessity and Preservation of Personal Protective Equipment. AAPM&R Position Statement on the Necessity and Preservation of Personal Protective Equipment
- Dowman L, Hill CJ, Holland AE (2014) Pulmonary rehabilitation for interstitial lung disease. Cochrane Database Syst Rev.
- Burtin C, Saey D, Saglam M (2012) Effectiveness of exercise training in patients with COPD: the role of muscle fatigue. Eur Respir J 40: 338–344.
- Hui DS, Joynt GM, Wong KT (2005) Impact of severe acute respiratory syndrome (SARS) on pulmonary function, functional capacity and quality of life in a cohort of survivors. Thorax 60: 401–409.
- Xie L, Liu Y, Xiao Y(2005) Follow-up Study on Pulmonary Function and Lung Radiographic Changes in Rehabilitating Severe Acute Respiratory Syndrome Patients After Discharge. Chest 127: 2119–2124.
- Venkataraman T, Frieman MB (2017) The role of epidermal growth factor receptor (EGFR) signaling in SARS coronavirus-induced pulmonary fibrosis. Antiviral Res 143: 142–150.
- Ngai JC, Ko FW, Ng SS, To KW, Tong M et al. (2010) The long-term impact of severe acute respiratory syndrome on pulmonary function, exercise capacity and health status. Respirology 15: 543–550.
- Jenkins S, Čečins N (2011) Six-minute walk test: observed adverse events and oxygen desaturation in a large cohort of patients with chronic lung disease. Intern Med J 41: 416–422.
- Vogiatzis I, Zakynthinos S (2012) Factors limiting exercise tolerance in chronic lung diseases. Compr Physiol 2: 1779–1817.
- Boutou AK, Pitsiou GG, Trigonis I (2011) Exercise capacity in idiopathic pulmonary fibrosis: the effect of pulmonary hypertension. Respirology 16: 451–458.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences