Specificity and Sensitivity of NIPT for Prenatal Screening of Down Syndrome in 100 Pregnant Women from Tonekabon, Iran
Mohammad Akbari, Seyed Hashem Mirmazloumi, M Garshasbi, Zahra Sadat Talari and Fariba Sadeghi
DOI10.21767/2471-299X.1000066
Mohammad Akbari1, Seyed Hashem Mirmazloumi2, M Garshasbi3, Zahra Sadat Talari4 and Fariba Sadeghi1*
1Department of Medical School, Islamic Azad University, Tonekabon, Mazandaran, Iran
2Medical Genetics, Cytogenetic Unit, DeNA Genetic Laboratory, Tehran, Iran
3Department of Medical Genetics, School of Medical Sciences, Tarbiat Modares University, Tehran, Iran
4Faculty of Biological Sciences and Biotechnology, Shahid Beheshti University, Tehran, Iran
- *Corresponding Author:
- Fariba Sadeghi
Assistant Professor, Department of Medical School, Faculty of Medical Sciences
Islamic Azad University, Tonekabon, Mazandaran, P.O. Box: 46841-61167, Iran
Tel: 00981154230513-5
Fax: 00981154224409
E-mail: khazarson@gmail.com
Received date: February 17, 2018; Accepted date: March 16, 2018; Published date: March 23, 2018
Citation: Akbari M, Mirmazloumi SH, Garshasbi M, Talari ZS, Sadeghi F (2018) Specificity and Sensitivity of NIPT for Prenatal Screening of Down Syndrome in 100 Pregnant Women from Tonekabon, Iran. Med Clin Rev. 4:3. doi: 10.21767/2471-299X.1000066
Copyright: © 2018 Akbari M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Down syndrome is one of the most common genetic disorders, with a prevalence of one in 600 live births. There are numerous methods for diagnosis of this syndrome before birth such as non-invasive prenatal testing (NIPT). This test evaluates positive and negative predictive values of Down syndrome screening as well as determining the gender of the fetus. Data were collected from 100 pregnant women who visited obstetrics and gynecology clinic of Tonekabon Hospital, Tonekabon, Iran. The average age of pregnant women was 35.9 and the average gestational age was 12 to 13 weeks. About 40% of participating mothers had a history of previous pregnancies (32%), 45% of mothers had no history of live births and none of them had a family history of developing Down syndrome. According to the results, 56 percent of babies were male and 44 percent were female and none of the fetuses had Down syndrome. Results of the present study also indicated that NIPT sensitivity and specificity in the diagnosis of Down syndrome and also the baby's gender were 100%. The positive and negative predictive values were also 100% as well. This study has shown that NIPT as a diagnostic test is used to detect Down syndrome in all pregnancies, including high-risk pregnancies such as cases with high maternal age. Another important issue which has to be taken into account is a source of support such as Insurance coverage for the test.
Keywords
Down syndrome; NIPT; False positive; NT; Sensitivity; Specificity
Introduction
Down syndrome is one of the most common genetic disorders with mental and physical symptoms such as learning difficulty and developmental delay [1,2]. Down syndrome occurs in approximately one in 600 births. There are numerous methods for screening and diagnosis of Down syndrome during pregnancy. Nowadays, pregnant women are undergoing ultrasonography for evaluating the thickness of nuchal translucency thickness in their 11th to 14th weeks of pregnancy. Nuchal fold is usually thicker in fetuses with Down syndrome compared to normal ones. During the first trimester of pregnancy, blood tests are conducted to check Down syndrome, but unfortunately, false positive results seem to be inevitable in blood tests. Therefore, in case of further tests are required in order to become certain about the diagnosis [3,4]. Detecting Down syndrome is crucial and using non-invasive methods with high sensitivity can be useful to identify the syndrome eliminating the risk of miscarriage. Non-invasive prenatal testing (NIPT) is used for screening of fetal chromosomal abnormalities [5]. Fetal cell-free DNA which is found in mother's plasma is the basis of this analytic test [2,6]. NIPT enables us to identify fetal chromosomal trisomies of chromosomes 13, 18, 21, X and Y, it also helps to identify monosomy of chromosome X. NIPT sensitivity for Trisomies 21, 18 and 13 is estimated with 99%, 97%, and 79% respectively. Furthermore, the probability of false positive X trisomy and monosomy is 1%. Abnormal need further evaluations to be confirmed since NIPT is a screening test. Development of experimental techniques and also a larger group of mothers will improve specificity and sensitivity of the test. Therefore, this test is predicted to become the primary assessment tool for screening of common trisomies and will eradicate the need for invasive tests in the near future [7].
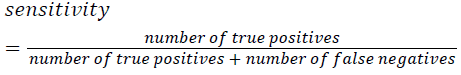
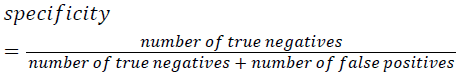
Materials and Methods
This is a diagnostic study that was performed in a retrospective form. 100 pregnant women with gestational age of 11 to 18 weeks, who had visited Genetic laboratories that provided NIPT, from 2014 to 2016, were selected randomly and enrolled in the study. Data was collected from these 100 mothers who visited gynecology and obstetrics clinic in Tonekabon Hospital, Tonekabon, Iran. NIPT sensitivity, specificity, positive predictive value and negative predictive value were calculated by means of the respective formula, to separately diagnose Down syndrome and determine Fetus gender using software STATA (version 13). Patients with NT values over 2.5 between weeks 11 and 13 were excluded from the present study. To determine CRL (Crown-rump length) and NT between weeks 11 and 13; patients with NT value less than 2.5, were enrolled in our study. Mothers with a history of Down syndrome and multiple pregnancies were excluded from this study. Participants were informed about NIPT and after they signed consent forms about 10 ml of venous blood was drawn for the test. Complete blood samples were centrifuged with dual centrifuge protocol at 1600 rpm for 10 minutes at. In the next step, the supernatant was transferred to a 2 ml sterile Eppendorf tube in -18. Afterwards, it was centrifuged at 1600 RPM at 4°C for 10 minutes. The final supernatant was transferred to a new Eppendorf tube that was maintained temporarily in dry ice without further processing. All molecular procedures including DNA isolation, library construction and sequencing was performed in the Clinical Laboratory of Beijing Genomic Institute (BGI), Shenzhen, China with confirmation number ISO/IEC 17025. All plasma samples were frozen and molten only once. The report included evaluating the risk of trisomy 13, 18 and 21.
Results
Data were categorized based on low risk or high risk, the gender of the fetus, maternal age, the number of pregnancies and family history of Down syndrome. Finally, the results were analyzed and compared (Tables 1 and 2).
| Frequency | Percent | Cumulative frequency | ||
|---|---|---|---|---|
| Age group | <25 | 0 | 0 | 0 |
| 25-29 | 10 | 10.0 | 10.0 | |
| 30-34 | 25 | 25.0 | 35.0 | |
| 35-39 | 42 | 42.0 | 77.0 | |
| 40< | 23 | 23.0 | 100.0 | |
| Total | 100 | 100.0 | - | |
| Age average | 35.90 | 4.356 | ||
Table 1: Distribution of participants according to age groups.
| Frequency | Percent | Cumulative frequency | ||
|---|---|---|---|---|
| Pregnancy week | 11 | 13 | 13 | 13 |
| 12 | 20 | 20 | 33 | |
| 13 | 20 | 20 | 53 | |
| 14 | 8 | 8 | 61 | |
| 15 | 11 | 11 | 72 | |
| 16 | 9 | 9 | 81 | |
| 17 | 7 | 7 | 88 | |
| 18 | 12 | 12 | 100 | |
| Total | 100 | 100 | - | |
| Average of pregnancy weeks | 13.99 | 2.229 | ||
Table 2: Distribution of participants according to their gestational age.
Gender of the fetuses, sensitivity-specificity, positive predictive value and negative predictive value were determined. None of the participating mothers underwent amniocentesis, thus the gold standard for comparison and approval of the results was the newborn baby itself. Those with positive results underwent amniocentesis and their results were recorded (Table 3).
| Main variable | Subcomponent | Frequency | Percent | Cumulative frequency |
|---|---|---|---|---|
| Gender by NIPT | Male | 56 | 56 | 56 |
| Female | 44 | 44 | 100 | |
| Real gender of baby after birth | Male | 56 | 56 | 56 |
| Female | 44 | 44 | 100 | |
| Down syndrome | No | 100 | 100 | 100 |
| Yes | 0 | 0 | 100 | |
| History of mother's IVF | No | 93 | 93 | 93 |
| Yes | 7 | 7 | 100 | |
| Patao syndrome | No | 100 | 100 | 100 |
| Yes | 0 | 0 | 100 | |
| Edward syndrome | No | 100 | 100 | 100 |
| Yes | 0 | 0 | 100 |
Table 3: Distribution of participants according to clinical findings associated with NIPT.
Determination of NIPT sensitivity and specificity:
True positive: the patient is diagnosed patient correctly=zero percent
False positive: healthy person is diagnosed patients wrongly=zero percent
True negative: healthy people, are diagnosed healthy correctly=100 percent
False negatives: the patient is diagnosed healthy wrongly=zero percent
Discussion and Conclusion
Compared to other diagnostic tests, NIPT has higher sensitivity and specificity, less false positive and negative predictive values in the diagnosis of Down syndrome and sex determination. Unfortunately, in this study no positive cases were observed. Although this is normal for 100 samples (usually it is one out of 600), the authors cannot assess the sensitivity of NIPT according to this data. A Summary of different studies on Down syndrome screening tests and its diagnostic ability has been shown in Table 4.
| Method | Diagnosis ability | False positive | Pregnancy age | Nature of method |
|---|---|---|---|---|
| Screening with help of chemical markers of mother's blood | 70%-90% | 5% | 11-13+6 | Non-invasive |
| 15-20+6 | ||||
| NT ultrasonography | 60%-80% | 5% | 11-13+6 | Non-invasive |
| CVS | >99% | Zero | 10-13 | Invasive(1-4 percent risk of abortion) |
| Amniocentesis | >99.9% | Zero | 16-21 | Invasive(0.5-1 percent risk of abortion) |
| NIPT | 99.90% | 0.10% | From week 10 | Non-invasive |
Table 4: Comparison of screening method for Down syndrome.
According to the data, it can be concluded that NIPT as a non-invasive diagnostic test has a better function compared to other tests including amniocentesis, CVS, NT ultrasonography and chemical markers screening. Its biggest advantage is that it is non-invasive and carries no risk of miscarriage. Moreover, just a few milliliters of mother’s blood is needed for the test. Advantages of NIPT include:
High sensitivity and specificity: Studies on large populations have shown more than 99 percent specificity and sensitivity.
Early detection: NIPT can be performed after the 10th week of pregnancy thus there is enough time to make a better decision. Till 2013 the indication to do NIPT was for high-risk pregnancies, but after 2014 based on guidelines of American College of Medical Genetics (ACMG) and Royal College of Obstetrics and Gynecology (RCOG) and also Professor Nicolaides’ recommendation, NIPT is becoming a common screening test with high sensitivity [8-10].
Acknowledgement
Patients who underwent this study and DeNA Genetic Laboratory, Tehran, Iran are highly acknowledged.
References
- Cohen WI (2003) Health care guidelines for individuals with Down syndrome-1999 revision. Down Syndrome 237.
- Newberger DS (2000) Down syndrome: Prenatal risk assessment and diagnosis. Americ Fam Phys 62: 825-832.
- Benn P, Borrell A, Cuckle H, Dugoff L, Gross S, et al. (2012) Prenatal detection of Down syndrome using massively parallel sequencing (MPS): A rapid response statement from a committee on behalf of the Board of the International Society for Prenatal Diagnosis. Prenat Diagn 32: 1-2.
- Natoli JL, Ackerman DL, McDermott S, Edwards JG (2012) Prenatal diagnosis of Down syndrome: A systematic review of termination rates. Prenat Diagn 32: 142-153.
- Lau TK, Jiang F, Chan MK, Zhang H, Salome Lo PS, et al. (2013) Non-invasive prenatal screening of fetal Down syndrome by maternal plasma DNA sequencing in twin pregnancies. J Maternal-Fetal Neonat Med 26: 434-437.
- Twiss P, Hill M, Daley R, Chitty LS (2014) Non-invasive prenatal testing for Down syndrome. Semin Fetal Neonat Med 19: 9-14.
- Norton ME, Brar H, Weiss J, Karimi A, Laurent LC, et al. (2012) Non-invasive chromosomal evaluation (NICE) study: Results of a multicenter prospective cohort study for detection of fetal trisomy 21 and trisomy 18. Ameri Obstet and Gynec 207: 137.
- Schendel RV, Dondorp WJ, Timmermans DR, Hugte EJ, Boer A, et al. (2015) NIPTÃÆâÃâââ¬ÃâÃÂbased screening for Down syndrome and beyond: What do pregnant women think? Prenat Diagn 35: 598-604.
- Smith M, Lewis KM, Holmes A, Visootsak J (2014) A case of false negative NIPT for Down syndrome-lessons learned. Case Rep Gene 2014.
- Taylor JB, Chock VY, Hudgins L (2014) NIPT in a clinical setting: An analysis of uptake in the first months of clinical availability. J Gene Counsel 23: 72-78.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences
