Temperature Gradient Achieved in the Shoulder Area as a Result of Cold-Air Cryotherapy Treatment
Jiri Kminek
Health Committee of the Dukla Prague Sports Club, Prague, Czech Republic
Published Date: 2024-06-17DOI10.36648/2471-299X.10.2.42
Jiří Kmínek*
Health Committee of the Dukla Prague Sports Club, Prague, Czech Republic
- *Corresponding Author:
- Jiří Kmínek
Health Committee of the Dukla Prague Sports Club, Prague,
Czech Republic,
E-mail: jikminek@gmail.com
Received date: May 17, 2024, Manuscript No. IPMCR-24-19101; Editor assigned date: May 20, 2024, PreQC No. IPMCR-24-19101 (PQ); Reviewed date: June 03, 2024, QC No. IPMCR-24-19101; Revised date: June 10, 2024, Manuscript No. IPMCR-24-19101 (R); Published date: June 17, 2024, DOI: 10.36648/2471-299X.10.2.42
Citation: Kmínek J (2024) Temperature Gradient Achieved in the Shoulder Area as a Result of Cold-Air Cryotherapy Treatment. Med Clin Rev Vol.10 No.2: 42.
Abstract
Background: The recommendation for tissue cooling in musculoskeletal injuries has been recognized for decades, leading to the development of various cooling techniques over time. Guidelines for their utilisation primarily rely on empirical evidence, as there is currently a lack of objective quantification regarding their efficacy. A possible common metric for cooling methods might be the maximum temperature reduction attained during their application.
Methods: Ten healthy volunteers received cold-air cryotherapy treatment on their shoulders for 9 minutes. Thermal images of both shoulders were captured before, immediately after, 3 and 10 minutes post-therapy. The images were then analysed to assess temperature reduction, and the findings were compared with existing clinical data.
Results: Statistical analysis revealed a significant difference in temperature gradients between the treated and untreated shoulder during all post-cryotherapy measurements. The temperature reductions of 15.85°C, 11.55°C and 6°C immediately after, 3 minutes after and 10 minutes after cryotherapy application respectively, surpass existing clinical evidence, underscoring the cold air cryotherapy device in cooling efficacy.
Conclusion: The current study reaffirmed the efficacy of the cold air cryotherapy device when manually applied to the shoulder area, highlighting its potential in injury treatment, prevention and post-performance recovery.
Keywords
Cold-air therapy; Cryotherapy; Upper-limb injury; Shoulder treatment; Cooling effect; Thermal profile
Introduction
The beneficial effects of cold therapy have been recognized since ancient times, with Hippocrates noting the efficacy of snow and ice in reducing swelling. The recommendation to use ice for musculoskeletal injuries emerged in the 1960’s, followed by its recognized ability to mitigate secondary muscle injury in athletes in the 1970’s [1]. Over time, the physiological mechanisms underlying the effects of cold on injured tissue have been elucidated. One of the primary physiological responses to cold application is the activation of the sympathetic vasoconstrictive reflex, leading to reduced blood flow, which in turn diminishes edema and slows the delivery of inflammatory mediators, thereby decreasing inflammation in the affected area. Additionally, cold therapy is known to alleviate local pain through a process known as cold-induced neurapraxia, which lowers the activation threshold of tissue nociceptors and reduces nerve signal conduction velocity, thus mitigating pain. Furthermore, the reduction in metabolism and inhibition of the spinal cord reflex loop induced by cold therapy may help prevent secondary hypoxic damage and reduce muscle spasms, respectively [2].
While traditional cooling methods like ice packs and cold water immersion remain prevalent, particularly in sports medicine, newer techniques are gaining traction in post-injury and postoperative rehabilitation and prevention. Whole Body Cryotherapy (WBC) is emerging as a versatile tool for treating and preventing various health conditions, including multiple sclerosis and arthritis, and is becoming an integral component of regenerative sports programs. Whole Body Cryotherapy (WBC) involves exposing individuals to extreme temperatures for up to 4 minutes, typically utilising liquid nitrogen or refrigerated cold air that can exceed -100°C [3,4]. Alongside WBC, other methods like Partial Body Cryotherapy (PBC) and Local Cryotherapy (LC) are gaining prominence. PBC involves subjecting the individual to the same cooling conditions as WBC but without exposing the head, while LC targets specific local areas with low temperatures. LC encompasses various cooling methods applied locally, with modern technological trends focusing on cryotherapy units that utilise cooling gases such as cold air, carbon dioxide microcrystals and liquid nitrogen vapours [4].
Although cooling methods vary widely in terms of exposure time, cooling medium temperature, and number of applications, with durations ranging from 2 to 20 minutes, temperatures ranging from 0°C-195°C, and the number of sessions ranging from 1 to 20, there is currently no standardized method or consensus for quantifying their effectiveness [4,5]. The recommendations for using cooling methods are predominantly based on empirical experience, as objective quantification of their effectiveness is currently lacking [2].
A potential unifying indicator for cooling methods could be the maximum temperature reduction achieved during their application. Existing clinical evidence shows that these values vary considerably, ranging from 6.76°C for cold-air cryotherapy to 12.1°C for WBC [4-8].
The objective of the present study is to assess the temperature reduction achieved through the application of a cold-air cryotherapy unit specifically targeting the shoulder area. This region often necessitates cold therapy for various health limitations, yet there is insufficient clinical evidence concerning the attainment of the target temperature, particularly with devices utilising cold-air cryotherapy.
Materials and Methods
The temperature profile evaluation was conducted as part of an experimental treatment involving healthy volunteers in April 2024. Although previous research indicated that a minimum sample size of 2 subjects was required to detect a significant (p<0.05) difference with 80% power, 10 volunteers were gradually recruited for this study [9]. Participants with contraindicated conditions such as Raynaud's disease, cold hypersensitivity (cold urticaria), open wounds (including burns), cardiovascular and blood perfusion disorders, skin sensitivity disorders, advanced diabetes mellitus, spinal cord injury, acrocyanosis, vascular inflammation, systemic lupus erythematosus, cold-induced bronchospasm, or any haematological disorder affecting blood clotting were excluded. Additionally, individuals with ongoing infections, menstruation in women, any ongoing medication use, or upper limb injuries within the last 2 years were also excluded due to potential influences on the body's thermal profile. The research adhered to the principles outlined in the declaration of Helsinki, and all volunteers were fully informed about the procedures, associated risks, and potential publication of the results [10]. They provided their consent by signing an informed consent form before participating in the study.
To minimise the impact of environmental factors on the participants' body temperature, the temperature and humidity levels in the treatment room were carefully regulated, maintaining parameters within a range of 21°C ± 1°C and 50%, respectively. Each participant was instructed to rest uncovered on a sofa for 20 minutes prior to therapy initiation to allow for stabilisation of their body temperature. Thermal imaging was conducted using a Fluke Ti32 thermal camera (Fluke Corporation, Everett, Washington) with features compliant with medical standards and guidelines for infrared imaging. The camera settings included an emissivity value set at 0.98, sensitivity of ≤ 45 mK NETD, spectral range of 8-14 μm, resolution of 320 × 240 pixels, spatial resolution of 2.5 mRad IFOV at a distance of 7.5 cm from the detector, and accuracy of ± 2°C or 2%. The camera was activated at the commencement of the 20-minute stabilisation period and calibrated prior to measurement.
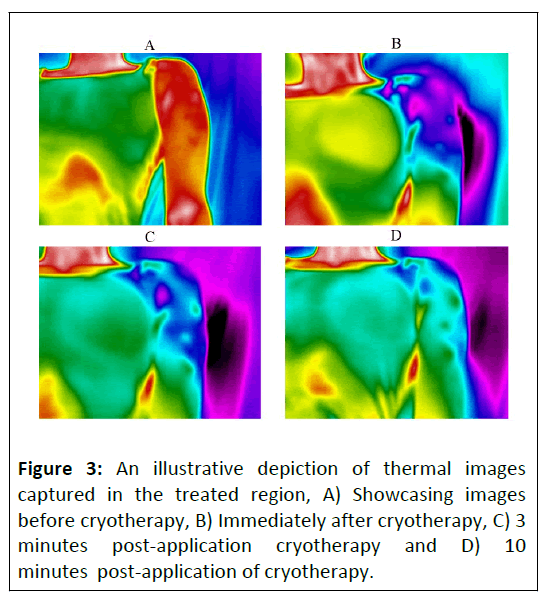
The shoulder area was subjected to cold therapy using a cryotherapy unit (BTL Industries, Ltd.). The therapy was manually applied using a cooling hose (ø15 mm nozzle), with the intensity adjusted based on the subject's feedback to ensure a cooling effect without causing tissue damage. The therapy duration was 9 minutes. An example of therapy is shown in Figure 1. Thermal images of both the treated and untreated shoulders were captured immediately before and after the commencement of therapy, as well as 3 and 10 minutes post-therapy. The thermal images were processed and analysed using the Fluke Smartview 4.3 program (Fluke Corporation, Everett, Washington), followed by further statistical evaluation using a custom-written script in Matlab R2023a (MathWorks Inc., Natick, Massachusetts). Thermal profiles were generated by analysing temperatures along a straight line across the observed area. As the data did not follow a normal distribution based on the Shapiro-Wilk test, nonparametric tests were employed for statistical analysis. Specifically, the Wilcoxon Signed Rank test was used to compare pre- and post-treatment temperatures, and the Mann-Whitney U test was utilised to compare data between the treated and untreated limbs. A significance level of p<0.05 was considered statistically significant. Values are presented as medians with Inter Quartile Range (IQR).
Results
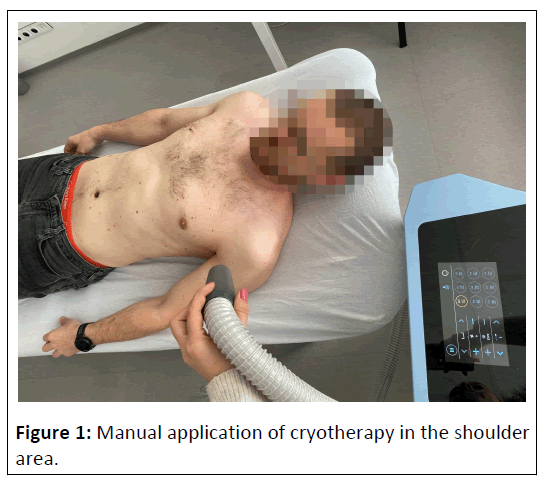
Temperature values measured during individual time intervals are summarised in Table 1. In the treated shoulder, a clear trend of temperature decrease due to cryotherapy application is observed in all volunteers, followed by a gradual increase, which still shows significant changes compared to the original value even after ten minutes. Only slight temperature fluctuations are observed in the untreated limb, likely due to the close proximity of cold applications. The temperature courses are visualised in Figure 2.
| S.no. | Subject | Before | After | After 3 min | After 10 min | ||||
|---|---|---|---|---|---|---|---|---|---|
| Treated | Untreated | Treated | Untreated | Treated | Untreated | Treated | Untreated | ||
| 1 | Median | 35.7 | 35.3 | 22.1 | 35.2 | 25 | 34.4 | 29.1 | 34 |
| IQR | 0.6 | 1.4 | 0.3 | 0.1 | 0.6 | 0.8 | 0.7 | 0.5 | |
| 2 | Median | 34.2 | 34.7 | 20.9 | 33.3 | 25 | 34.9 | 29.3 | 34.7 |
| IQR | 1.1 | 1.5 | 0.6 | 0.5 | 0.2 | 0.3 | 0.8 | 0.7 | |
| 3 | Median | 34.7 | 34.7 | 13.9 | 34.9 | 22.5 | 34.8 | 29 | 34.5 |
| IQR | 0.7 | 0.8 | 1.1 | 2.5 | 0.4 | 2.6 | 1.4 | 1.8 | |
| 4 | Median | 34.6 | 34.5 | 18.2 | 35.1 | 23.3 | 35.5 | 27.6 | 35.2 |
| IQR | 0.4 | 0.3 | 1.3 | 0.5 | 0.7 | 0.7 | 1 | 1.2 | |
| 5 | Median | 35.8 | 36.1 | 18.1 | 35.5 | 25.4 | 35.3 | 29 | 35.2 |
| IQR | 0.2 | 1 | 0.4 | 0.7 | 0.3 | 0.6 | 0.4 | 1.5 | |
| 6 | Median | 35.3 | 36 | 19.3 | 35.2 | 21 | 35 | 28.4 | 34.8 |
| IQR | 0.9 | 0.4 | 0.4 | 1.3 | 0.5 | 0.8 | 0.9 | 0.7 | |
| 7 | Median | 34.5 | 34.7 | 19 | 34.4 | 23.3 | 35.2 | 28.6 | 35.2 |
| IQR | 0.7 | 0.3 | 1.3 | 0.4 | 0.9 | 0.2 | 0.3 | 0.3 | |
| 8 | Median | 34.6 | 34.4 | 19.7 | 33.2 | 25.1 | 34.9 | 28.8 | 34.5 |
| IQR | 0.6 | 0.1 | 0.8 | 1.3 | 1.1 | 1.7 | 0.7 | 1.6 | |
| 9 | Median | 35.7 | 35.4 | 15.4 | 34.3 | 22.1 | 34.4 | 29.2 | 35.4 |
| IQR | 0.7 | 0.9 | 1.4 | 0.6 | 1.1 | 1.4 | 0.9 | 1 | |
| 10 | Median | 35.9 | 36 | 20.4 | 35.9 | 23.6 | 35.1 | 29.3 | 35.2 |
| IQR | 0.8 | 0.2 | 0.3 | 0.2 | 0.8 | 0.4 | 1.2 | 1.2 | |
Table 1: Summary of median temperatures measured across the treated and untreated shoulder before initiation of cryotherapy (Before), immediately after termination of therapy (After), 3 minutes (After 3 min) and 10 minutes after termination of cold application (After 10 min).
A statistical analysis comparing the temperature values of treated and untreated limbs revealed that despite the initial temperatures being almost identical, the differences measured immediately after, 3 minutes after, and even 10 minutes after the application of cryotherapy reached statistical significance with p<0.001 (Table 2).
| Treated | Untreated | P (Mann-Whitney U test) | ||
|---|---|---|---|---|
| Before | Median | 35 | 35 | 0.644 |
| IQR | 0.8 | 1.1 | ||
| After | Median | 19.15 | 35 | <0.001 |
| IQR | 0.85 | 1.05 | ||
| 3 Mins | Median | 23.45 | 34.95 | <0.001 |
| IQR | 0.8 | 0.75 | ||
| 10 Mins | Median | 29 | 35 | <0.001 |
| IQR | 0.9 | 1 | ||
Table 2: Statistical analysis comparing the median measured temperatures for the treated and untreated limbs at each measurement point. Values of p<0.05 are deemed statistically significant.
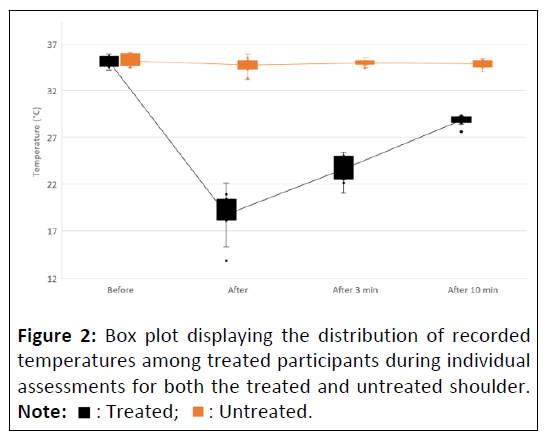
A comparison of the temperature changes achieved across the treated and untreated areas revealed that while the treated area exhibited statistically significant differences between the initial temperatures and the temperatures measured after the application of cryotherapy, no statistically significant change was observed in the untreated area during any time interval (Table 3). Figure 3 illustrates the visual contrast in temperature distribution across the cooled area during individual measurement points.
| Treated | Untreated | |||
|---|---|---|---|---|
| ΔT | P (Wilcoxon sign rank test) | ΔT | P (Wilcoxon sign rank test) | |
| Before vs. After | 15.85 | 0.004 | 0 | 0.059 |
| Before vs. 3 M | 11.55 | <0.001 | 0.05 | 0.449 |
| Before vs. 10 M | 6 | <0.001 | 0 | 0.195 |
Table 3: Statistical assessment of temperature variances observed during individual measurements for the treated and untreated shoulder. Values of p<0.05 are deemed statistically significant.
Discussion
The current study observed a significant reduction in shoulder temperature by more than 15°C following a nine-minute cold-air cryotherapy session maintaining statistical significance even ten minutes after the end of cooling, proving the abovestandard cooling efficacy outlined in existing clinical literature. This finding holds promise for the effective management of upper limb conditions. Notably, research on temperature reduction during cold therapy predominantly focuses on lower limb applications, particularly knees and ankles, making investigations into upper limb treatment relatively unique.
Cold therapy has shown effectiveness in post-injury and postoperative rehabilitation for upper limb conditions. For instance, Speer, et al. demonstrated the benefits of chilled water cryo cuff in postoperative shoulder recovery, specifically following procedures such as anterior shoulder stabilisation, rotator cuff repair, or total shoulder replacement [11,12]. Research conducted by Bishop, et al. on college baseball players demonstrated the benefits of cold therapy in reducing fatigue and expediting recovery during sports performance. Cryotherapy, in the form of ice bags, resulted in attenuated velocity loss during baseball pitching, decreased rating of perceived exertion, and facilitated subjective recovery during a simulated game [13]. In a study by El-Maksoud, et al. involving children with cerebral palsy, the effectiveness of cold gel packs in reducing spasticity and improving hand function was investigated. The study revealed that combining cold therapy with conventional physical and occupational therapy resulted in superior outcomes compared to relying solely on conventional therapy [14]. Cold therapy is widely employed across various medical, rehabilitative, and sports contexts, employing diverse modalities and protocols. Among these, the cold-air cryotherapy device stands out as a relatively recent innovation, offering rapid and convenient cold application without necessitating consumables. Despite its potential benefits, robust clinical evidence elucidating its effectiveness and underlying mechanisms, particularly in upper limb applications, remains limited. The assessment of the temperature gradient attained during therapy holds promise for its expanded application in physiotherapy practice. This modality has demonstrated the ability to swiftly and effectively reduce the temperature of the treated area to levels conducive to clinical efficacy. The observed reduction in skin temperature in the treated area following cryotherapy application is notably remarkable within the context of existing evidence on cold-air cryotherapy, surpassing even methods employing other cooling modalities [4-8]. The subsequent rise in tissue temperature post-therapy aligns with the trend observed in whole body cryotherapy at -110°C and cold water immersion at 8°C, as presented by Costello, et al. [7].
This study should be viewed as a preliminary assessment of temperature distribution across the shoulder area, considering its inherent limitations. An area for potential improvement lies in conducting multiple therapy sessions for each subject, as well as measuring temperature at various depths within the tissue. This would provide more detailed and accurate information about the therapeutic effects. Additionally, conducting repeated therapies would help minimise the influence of environmental factors on body temperature. Furthermore, focusing on a healthy population limits the evaluation of effectiveness within specific rehabilitation contexts, necessitating separate trials for such purposes. Despite these limitations, the findings of this study offer promise for future research into potential clinical applications.
Conclusion
The recent study has affirmed the efficacy of the cold-air cryotherapy device in lowering shoulder area temperatures. The attained temperature reduction surpassed 15°C and exhibited a statistically significant decrease even up to 10 minutes postcryotherapy. These results underscore the method's potential in injury management, as well as post-performance sports recovery.
References
- Kwiecien SY, McHugh MP (2021) The cold truth: The role of cryotherapy in the treatment of injury and recovery from exercise. Eur J Appl Physiol 121: 2125-2142.
[Crossref], [Google Scholar], [Indexed]
- Malanga GA, Yan N, Stark J (2015) Mechanisms and efficacy of heat and cold therapies for musculoskeletal injury. Postgrad Med 127: 57-65.
[Crossref], [Google Scholar], [Indexed]
- Allan R, Malone J, Alexander J, Vorajee S, Ihsan M, et al. (2022) Cold for centuries: A brief history of cryotherapies to improve health, injury and post-exercise recovery. Eur J Appl Physiol 122: 1153-1162.
[Crossref], [Google Scholar], [Indexed]
- Hohenauer E, Costello JT, Stoop R, Küng UM, Clarys P, et al. (2018) Cold-water or partial-body cryotherapy? Comparison of physiological responses and recovery following muscle damage. Scand J Med Sci Sports 28: 1252-1262.
[Crossref], [Google Scholar], [Indexed]
- Savić M, Fonda B, Sarabon N (2013) Actual temperature during and thermal response after whole-body cryotherapy in cryo-cabin. J Therm Biol 38: 186-191.
- Costello JT, Donnelly AE, Karki A, Selfe J (2014) Effects of whole body cryotherapy and cold water immersion on knee skin temperature. Int J Sports Med 35: 35-40.
[Crossref], [Google Scholar], [Indexed]
- Costello JT, CulliganK, Selfe J, Donnelly AE (2012) Muscle, skin and core temperature after -110°C cold air and 8°C water treatment. PloS one 7: e48190.
[Crossref], [Google Scholar], [Indexed]
- Cholewka A, Stanek A, Wójcik M, Sieroń-Stołtny K, Drzazga Z (2017) Does local cryotherapy improve thermal diagnosis similar to whole-body cryotherapy in spinal diseases? J Therm Anal Calorim 127: 1155–1162.
- Kminek J (2023) Temperature reduction after cryotherapy through knee and ankle compression sleeves. J Clin Exp Orthopr 9: 403.
- Council of Europe (1997) Convention for protection of human rights and dignity of the human being with regard to the application of biology and biomedicine: Convention on human rights and biomedicine. Kennedy Inst Ethics J 7: 277-290.
- Amalu W (2018) International academy of clinical thermology medical infrared imaging standards and guidelines.
- Speer KP, Warren RF, Horowitz L (1996) The efficacy of cryotherapy in the postoperative shoulder. J Shoulder Elbow Surg 5: 62-68.
[Crossref], [Google Scholar], [Indexed]
- Bishop SH, Herron RL, Ryan GA, Katica CP, Bishop PA (2016) The effect of intermittent arm and shoulder cooling on baseball pitching velocity. J Strength Cond Res 30: 1027-1032.
[Crossref], [Google Scholar], [Indexed]
- Abd El-Maksoud GM, Sharaf MA, Rezk-Allah SS (2011) Efficacy of cold therapy on spasticity and hand function in children with cerebral palsy. J Adv Res 2: 319-325.
[Crossref], [Google Scholar]

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences
 : Treated;
: Treated;  : Untreated.
: Untreated.