The Utilisation of Psychiatry and Other Mental Health Benefits by Members of Medical Schemes, South Africa
Michael Mncedisi Willie
Council for Medical Schemes, South Africa
- *Corresponding Author:
- Michael Mncedisi Willie
Council for Medical Schemes, South Africa
E-mail: m.willie@medicalschemes.co.za
Received Date: September 30, 2020; Accepted Date: October 27, 2020; Published Date: November 03, 2020
Citation: Willie MM (2020) The Utilisation of Psychiatry and Other Mental Health Benefits by Members of Medical Schemes, South Africa. Med Clin Rev. Vol. 6 No. 5: 106
DOI: 10.36648/2471-299X.6.5.106
Abstract
Introduction: Section 24 (2) (e) of the Medical Schemes Act is very clear in that a medical scheme does: “not or will not unfairly discriminate directly or indirectly against any person on one or more arbitrary grounds, including race, gender, marital status, ethnic or social origin, sexual orientation, pregnancy, disability or state of health”.
Furthermore, section 9(4) of the Constitution is relevant and provides that: "No person may unfairly discriminate directly or indirectly against anyone on one or more grounds, including race, gender, sex, pregnancy, marital status, ethnic or social origin, colour, sexual orientation, age, disability, religion, conscience, belief, culture, language and birth."
Socioeconomic factors, inequalities, misdistribution of specialists’ services such as mental health and psychiatry services potentially result in some form of discrimination.
Objectives: The objective of this paper was to assess access to healthcare benefits paid to three medical service providers who are treating beneficiaries diagnosed with disabilities.
Setting: Medical schemes population, South Africa
Methods: The study utilized a cross-section design, using annual statutory returns data. The study mainly considered medical schemes claims data for psychiatrists and mental health related chronic conditions. The Entry and Verification criterion employed by the CMS (Council for Medical schemes) was employed to identify beneficiaries with chronic conditions. The analysis was conduction in SAS.9.4 (North Corlina).
Results: In this study, there were at the most 3 776 psychologists, and the median rate of benefit paid per event was R872 Interquartile range (IQR: R842-R916). The study also included a total of 620 psychiatrists and their median benefit paid per event was R1 119 (IQR: R1 013-R1 181). The number of psychologists was higher at 4.2 per 10 000 beneficiaries. It is still concerning that beneficiaries of medical schemes attracted co-payments as high as five percent (5%) for services such as a psychiatry benefit.
Conclusion: Inadequate access to benefits by beneficiaries of medical schemes with disabilities, as a consequence of poorly designed benefits, market forces and poor quality of care, also results in discrimination. Lastly, for psychiatrists, the government has to avail more training posts rather than merely increasing the salary of an individual psychiatrist.
Keywords
Prescribe minimum benefits; Disability; Mental health disorder; Chronic conditions; Medical schemes act
Introduction
Mental health and human rights
The human rights of people living with mental illness will be promoted and protected, through the active implementation of the Mental Health Care Act (2002). The inclusion of mental health in the Sustainable Development Goals represents a global commitment to including mental health among the highest health and development priorities for investment [1,2]. Between 76 percent and 85 percent of people with mental disorders receive no treatment for their disorder in low-middle income countries [3]. The Department of Health is committed to working with civil society and industry bodies to address the challenges facing people living with mental illnesses. The social and the economic impact of mental health cannot be overemphasised. Lund, Myer, Stein and Flisher [4] depicted that mental health accounts for just over 2 percent of South Africa’s GDP annually. The WHO (World Health Organisation), estimates the average annual costs of mental disorders for employees with depression to be 4.2 times higher than those incurred by a typical beneficiary (Table 1) [5].
Table 1 The Overall Economic Burden of Mental Disorders.
| Care costs | Productivity costs | Other costs | |
|---|---|---|---|
| Sufferers | Treatment and service fees/payments | Work disability, Lost earnings | Anguish/suffering treatment side-effects, suicide |
| Family and friends | Informal caregiving | Time off work | Anguish, isolation; stigma |
| Employers | Contributions to treatment and care | Reduced productivity | |
| Society | Provision of mental health care and general medical care, untreated illnesses (taxation/insurance) | Reduced productivity | Loss of lives, (unmet needs), social exclusion |
Disability and mental health
Defining disability, trivial as it may seem, is difficult because of the absence of a single unique definition that encompasses all aspects of disabilities. Disability is a component of mental illness, and, as a result, is a major contributor to the global burden of disease. Defining disability, trivial as it may seem, is difficult because of the absence of a single unique definition that encompasses all aspects of disabilities [6]. Many view disability as some loss of physical or mental functioning, while some define it as functional limitations or bodily impairments. Chaudhury, Deka and Chetia [7] conducted a study that looked at disability associated with mental disorders by analysing seven psychiatric disorders, namely, schizophrenia, bipolar mood disorder, anxiety disorders, depression, obsessive-compulsive disorder and dementia. These disorders were associated with significant disability, with schizophrenia being the most disabling.
Mental and substance use disorders
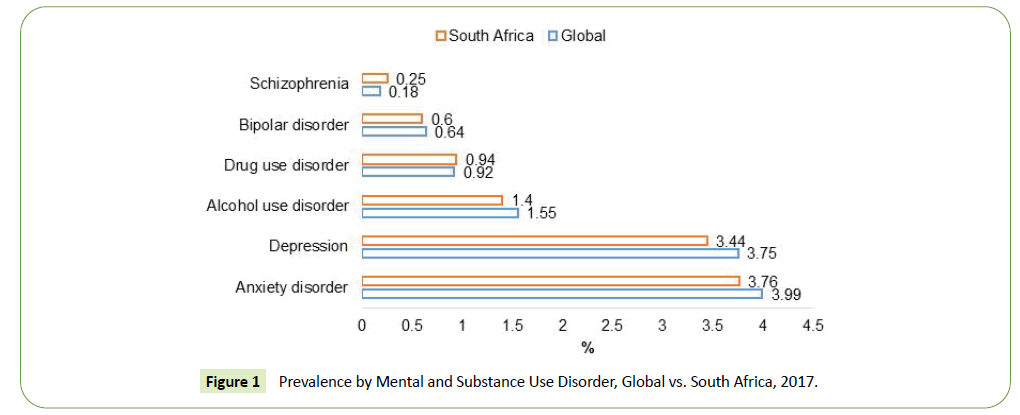
Depression is estimated at 3.75 percent for South Africa, compared to the global rate of 3.44 percent [8]. A Bipolar Mood Disorder (BMD) is estimated at 0.60 percent, compared to 0.64 percent globally [8]. Other studies have estimated the prevalence of bipolar mood disorder to be between 1 percent and 2 percent [9]. The IHE further estimates the prevalence of schizophrenia to be 0.18 percent, compared to the global rate of 0.25 percent (Figure 1).
Legislative requirement
The Medical Schemes Act, No. 131 of 1998 makes it mandatory for medical schemes to cover costs for the diagnosis, treatment or care of a defined set of benefits or Prescribed Minimum Benefits (PMBs), regardless of the benefit option members have selected. PMBs include any medical condition which meets the definition of an emergency, a limited set of 270 medical conditions and 26 chronic conditions defined in the Chronic Disease List (CDL).
The CDL specifies medication and treatment for the chronic conditions that are covered as PMBs. This law ensures that beneficiaries with chronic conditions are not risk-rated. Mental health conditions that are listed in the PMBs may qualify as mental health emergencies [10].
The following mental conditions that are listed in the PMBs may qualify as mental health emergencies:
• Acute delusional mood, anxiety, personality, perception disorders and organic mental disorder caused by drugs.
• Alcohol withdrawal delirium; alcohol intoxication delirium.
• Delirium: induced by; Amphetamine, Cocaine, or other psychoactive substances.
• Attempted suicide, irrespective of the cause.
• Brief reactive psychosis.
• Major affective disorders, including unipolar and bipolar depression.
• Schizophrenic and paranoid delusional disorders.
Strategic shift and priority focus on mental health-private sector
The effort to improve and prioritise mental health in the private sector is quite evident. As a result, numerous medical schemes are considering mental health as a priority strategic area. The government employees’ medical schemes annual report depicts mental health as a key component of benefit design enhancement [11]. Bonitas Medical Scheme (Bonitas) depicts Mental Health as a key priority and a key component of managed care services (Table 2) [12]. The CMS published Draft PMB definition guidelines in 2019 for mental health emergencies [10].
Table 2 Bonitas Medical Scheme Mental Health Managed Care Program.
| Mental health is a rapidly growing chronic condition in South Africa and is exacerbated by the stresses associated with socioeconomic challenges unique to the country. |
| Mental health features in the top five of Bonitas hospital admissions, and the associated cost increase has necessitated introducing a managed care approach to the condition. |
The guidelines focus on a set of recommendations for the diagnosis, treatment and care of individuals with a mental health emergency, in any clinically appropriate setting, as outlined in the Medical Schemes Act. Furthermore, the guidelines seek to improve clarity in respect of funding decisions by medical schemes, taking into consideration evidence-based medicine, affordability and, in some instances, cost-effectiveness.
Methods
Materials
The data used in this study were sourced from the annual statutory return submissions which schemes submit to the Office of the Registrar on an annual basis. The data were captured on the annual statutory returns system, then exported onto Microsoft Excel spread sheets prior to the analysis phase.
Setting
Data analysed included open and restricted schemes that were registered during the assessment period. The review period for the analysis was 2014-2018 period. Inclusion criteria were schemes that submitted complete data on the variables of interest.
Design
The study utilized a cross-section design, using annual statutory returns data. The study mainly considered medical schemes claims data for psychiatrists and mental health related chronic conditions.
Statistical analysis
The statistical analyses were performed using SAS software, version 9.4 (SAS Institute, North Carolina, US).
Results
Prevalence of Bipolar Mood Disorder (BMD) and Schizophrenia (SCZ)
Table 3 below depicts the prevalence of treated bipolar mood disorder (BMD) and schizophrenia (SCZ). The results reveal a prevalence of 4.36 per 1 000 beneficiaries for BMD and a prevalence of 0.53 per 1 000 beneficiaries for SCZ in 2018, this was higher for females than male beneficiaries. Over the period, the prevalence of BMD has increased by 88 percent. The prevalence of Schizophrenia (SCZ) has remained under 1 per 1000 between 2014 and 2018. However, there was a shift in the prevalence rate which increased by 27 percent over the review period. There was no notable difference between male and female beneficiaries.
Table 3 Prevalence in Bipolar Mood Disorder (BMD) and Schizophrenia (SCZ) - per 1 000 Beneficiaries.
| Chronic Code | Gender | 2014 | 2015 | 2016 | 2017 | 2018 |
|---|---|---|---|---|---|---|
| Bipolar Mood Disorder | Female | 4,37 | 5,01 | 5,01 | 5,26 | 5,49 |
| Male | 2,43 | 2,81 | 2,84 | 2,98 | 3,07 | |
| Total | 3,45 | 3,97 | 3,98 | 4,18 | 4,36 | |
| Schizophrenia | Female | 0,47 | 0,51 | 0,46 | 0,48 | 0,51 |
| Male | 0,49 | 0,54 | 0,51 | 0,54 | 0,55 | |
| Total | 0,48 | 0,52 | 0,48 | 0,51 | 0,53 |
Average growth of CDLs
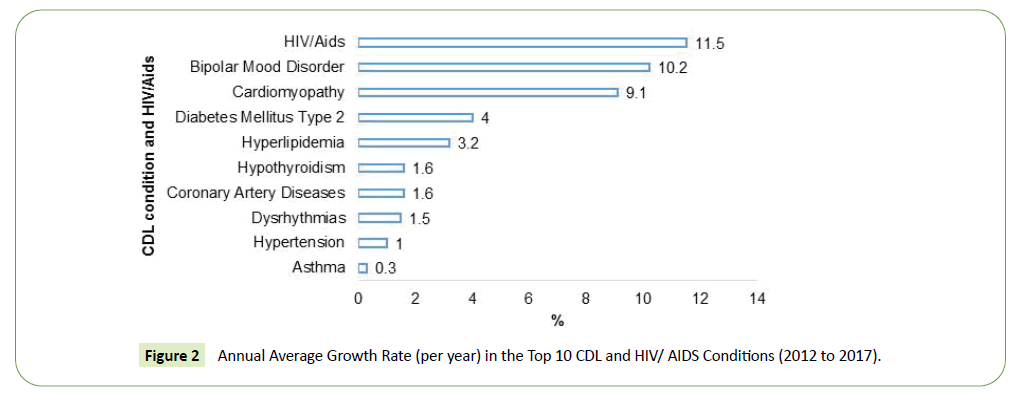
Figure 2 depicts the annual average growth rate (per year) in the top 10 CDL over the past 6 years. The important feature of the data is that BMD was ranked second after HIV, thus increasing at a higher rate. According to Figure 2, HIV/AIDS has been the fastest increasing condition, followed by BMD, with the average growth rate of these CDLs being above 10% per year.
Average expenditure per event for BMD and SCZ
The average cost of treating females diagnosed with BMD is nearly three times more than that of males. The average expenditure per event for male beneficiaries diagnosed with BMD was R7 100 and R2 126 per female beneficiary, respectively. Expenditure for an in-hospital event for male and female beneficiaries diagnosed with SCZ was R21 174 and R23 861 per beneficiary, respectively. The average expenditure for SCZ was generally higher than that of BMD (Table 4).
Table 4 Average Expenditure per Treated Beneficiary (BMD and SCZ).
| SCZ | |||
|---|---|---|---|
| Setting | Female | Male | All |
| In-hospital | 21 174 | 23 861 | 22 705 |
| Out-of-hospital | 7 115 | 8 687 | 7 904 |
| Grand Total | 10 027 | 12 561 | 11 339 |
| BMD | |||
| Setting | Female | Male | All |
| In-hospital | 7 100 | 2 126 | 5 077 |
| Out-of-hospital | 2 937 | 1 621 | 2 260 |
| Grand Total | 5 739 | 1 909 | 4 028 |
Benefits paid-psychiatry, psychology and social worker disciplines
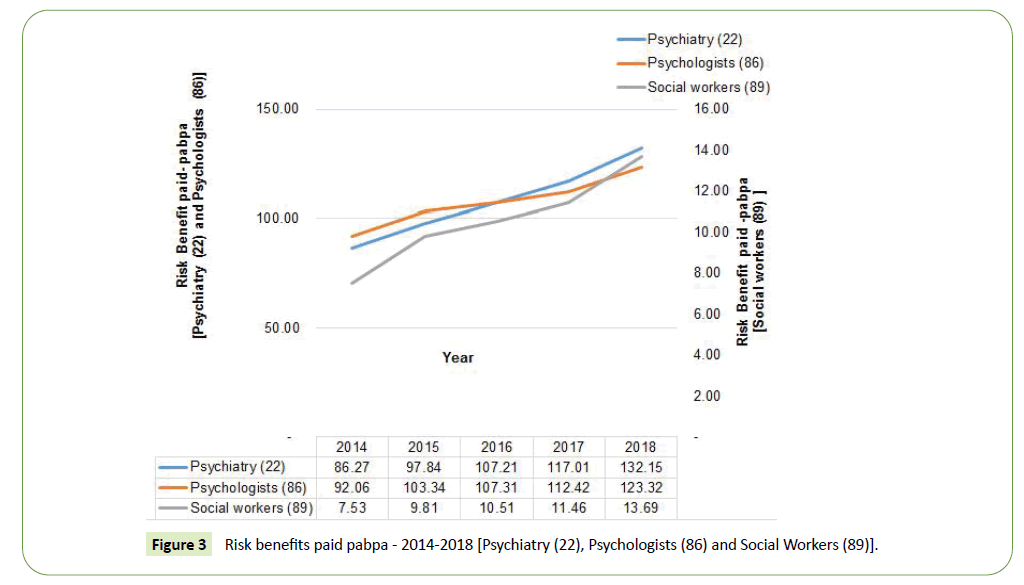
Risk benefits paid for mental related conditions accounted for more than 95 percent of the claimed amount in 2018. The rate of change in risk benefits paid between 2014 and 2018 was more pronounced in social workers (which increased by 82 percent), followed by psychiatry (which increased by 53 percent), and lastly the psychologists discipline (which increased by 34 percent). The average year on year increase was 17 percent, 12 percent and 8 percent respectively. The noteworthy feature of the data was the significant increases in psychiatry risk benefits, which were more pronounced in the last two years. The increase in psychiatry claims is possibly due to the increasing awareness of mental wellbeing and concerted efforts to remove the stigma around mental health issues and encouragement of those suffering to seek help. Furthermore, this could be seen as a reflection of the societal challenges that most beneficiaries are facing (Figure 3).
Discussion
There have been various developments regarding reprioritisation of mental health in the private health sector, and likewise developments in the public sector. The recent study by SADASG highlighted the challenges faced by members of medical schemes regarding cover [13]. One of the insights was that members who are affected by mental illness are in most instances, discriminated against by funders. In most instances, members are subjected to co-payments, and in others, inadequate cover of medications occurs. All this inadequacy, potentially, as a result, benefits the design and the reprioritisation of this condition and maximises cover. One of the main challenges is a shortage of providers insofar as access is concerned.
The recent publication by the CMS indicates a response to prioritise the provision of mental health and commitment of the private sector. There is however more that still needs to be done where benefit design is concerned. Major depressive disorder, bipolar disorder, schizophrenia, substances and psychiatric emergencies are all PMB conditions. However, only SCZ and bipolar disorder are included in the CDLs (Chronic Diseases List). One of the key findings of the study was the disparity in the health-seeking behaviour of male and female beneficiaries.
Chronic conditions such as BMD were more prevalent in females when compared to males. In some instances, the prevalence rate was nearly twice as high. A similar trend was noted regarding expenditure.
The other key finding revealed by the analysis was that admissions for health care facilities such as mental health institutions were more notable in young age bands such as 20-24 years and 40-45 years. This finding revealed that mental conditions are notable in both the young and the older working-class beneficiaries.
There has been a significant increase in the number of psychiatric beds in the private sector, over the past two decades. The distribution of the available beds seems to be the main challenge that needs to be prioritised; mainly due to the scarcity of human resources and the fact that only a handful of psychiatrists are available to both the insured and the uninsured population. Conclusion and Recommendations
Socio-economic and demographic factors
It is thus recommended that managed care programs should factor in the health-seeking behaviour between the types of beneficiaries, and that such program should also seek to encourage the male to be more pro-active in seeking health interventions. Thus, interventions by schemes and managed care programmes should also be targeted at specific age profiles, to make a significant impact, as a result of societal issues such as:
• Unemployment.
• Societal pressure such as dealing with pressure at work.
• Dealing with marital challenges such as divorce.
• Gender-based violence with its associated factors.
• Social issues such as substance abuse.
• There needs to be a focus on trauma.
Human resources
Both the private and the public sector need innovative solutions to attract more mental health professionals through training institutions thus producing more human resources for this important field. One of the innovative ways would be to look at the remuneration structure and review the funding model for increasing capacity in training facilities. Lastly, for psychiatrists, the government has to avail more training posts, rather than only increasing the salaries of individual psychiatrists.
Benefit design
It is concerning that mental disorders such as depression and anxiety are currently not covered as PMB. Thus, there is a need for a review of PMBs, particularly regarding conditions that are currently not covered. Therefore; the following is recommended: There should be a designated medical scheme designated provider arrangement to consider the scarcity of resources, insofar as access is concerned and the rules regarding co-payments should be reviewed.
It is concerning that some medical schemes are funding PMB related conditions such as mental health from the institutions’ savings accounts.
This should be prohibited and schemes that are non-compliant should be dealt with, as these types of scheme transfers run the risk of referring the funding of mental health back to the patients.
Acknowledgements
I would like to thank Martin Moabelo and Carrie-Anne Cairncross for their contribution in the development of this article.
Competing Interests
The authors have declared that no competing interest exist.
Authors’ Contributions
The author drafted the article, further input was received from Martin Moabelo and Carrie-Anne Cairncross.
Funding Information
This research article received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Disclaimer
The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of any affiliated agency of the author.
References
- Thornicroft G, Patel V (2014) Including mental health among the new sustainable development goals. BMJ 349: g5189.
- Sukeri K (2017) The National Mental Health Policy Framework & Strategic Plan 2013-2020: The Case of the Eastern Cape. South African Psychiatry 13: 16-19.
- Rathod S, Pinninti N, Irfan M, Gorczynski P, Rathod P, et al. (2017) Mental Health Service Provision in Low- and Middle-Income Countries. Health Serv Insights 10: 1178632917694350.
- Lund C, Myer L, Stein D, Williams DR, Flisher AJ (2013) Mental illness and lost income among adult South Africans. Soc Psychiatry Psychiatr Epidemiol 48: 845-851.
- World Health Organisation (WHO) (2003) Investing in MENTAL HEALTH. Geneva: World Health Organization.
- Tough H, Siegrist J, Fekete C (2017) Social relationships, mental health and wellbeing in physical disability: a systematic review. BMC Public Health 17: 414.
- Chaudhury PK, Deka K, Chetia D (2006) Disability associated with mental disorders. Indian J Psychiatry 48: 95-101.
- Institute for Health Metrics and Evaluation (IHME) (2018) Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2017 (GBD 2017) Results. Seattle, United States.
- Rowland TA, Marwaha S (2018) Epidemiology and risk factors for bipolar disorder. Ther Adv Psychopharmacol 8: 251‐269.
- www.medicalschemes.com
- https://www.gems.gov.za/en/
- Bonitas Medical Aid Schemes (Bonitas) (2019) Annual Integrated Report.
- Docrat S, Besada D, Cleary S, Daviaud E, Lund C (2019) Mental health system costs, resources and constraints in South Africa: a national survey. Health Policy and Planning 34: 706-719.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences