Surgical Management of Graft Redundancy after Colon Interposition for Esophageal Reconstruction
Abdelkader Boukerrouche
DOI10.21767/2471-299X.1000059
Abdelkader Boukerrouche*
Department of Digestive Surgery, Beni-Messous Hospital, University of Algiers, Algiers, Algeria
- *Corresponding Author:
- Boukerrouche A
Department of Digestive Surgery, Beni-Messous Hospital
University of Algiers, Algiers, Algeria
Tel: +213661227298
Fax: +21321931310
E-mail: aboukerrouche@yahoo.com
Received date: October 25, 2017; Accepted date: November 08, 2017; Published date: November 13, 2017
Citation: Boukerrouche A (2017) Surgical Management of Graft Redundancy after Colon Interposition for Esophageal Reconstruction. Med Clin Rev. 3:17. doi: 10.21767/2471-299X.1000059
Copyright: © 2017 Boukerrouche A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Colon graft redundancy is the most common late complication after colon interposition for esophageal re construction. Redundancy leads to mechanical dysfunction of the interposed colon and may occur several decades after initial reconstructive surgery. Food and liquid retention in the redundant colon causes disabling symptoms and nutritional disorders. When lifestyle modifications fail, surgical correction is indicated to improve life quality and to prevent complication. We describe two cases of interposed colon graft redundancy which were surgically treated with a successful surgical technique to correct this complication.
Keywords
Colon interposition; Esophageal reconstruction; Redundancy; Surgical correction
Introduction
Although gastric interposition remains the first surgical technique used to establish gut continuity following esophagectomy [1,2]. However Colonic interposition is preferred by some surgeons for many advantages including include its long length and usually its excellent blood supply and its resistance to refluxed gastric juice acid. Over time, colon interposition has been become an effective surgical procedure to reconstruct the diseased esophagus either in benign and malignant condition with acceptable mortality and mortality and good functional results. However and as reported by studies, the functional outcome following colon interposition for esophageal reconstruction may be compromised by mechanical complications mainly redundancy which develop several decades after initial reconstructive surgery and may require surgical treatment in symptomatic patients [3-6]. We describe the management of two cases of colon graft redundancy developed after substernal colon interposition for esophageal caustic stricture which were treated with successful surgical technique.
Case 1
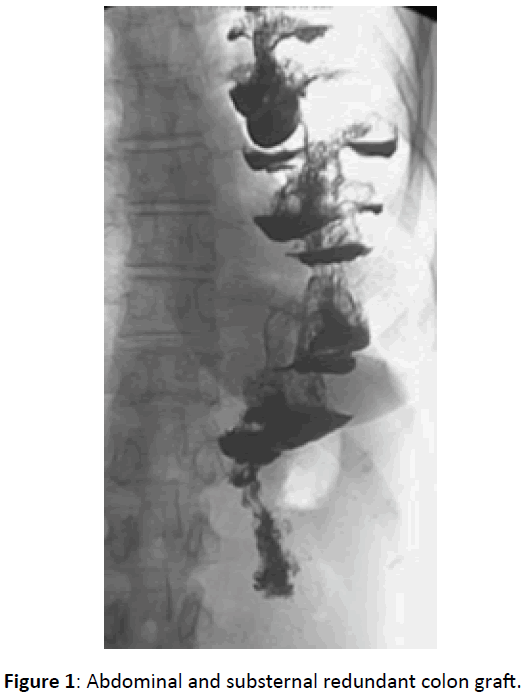
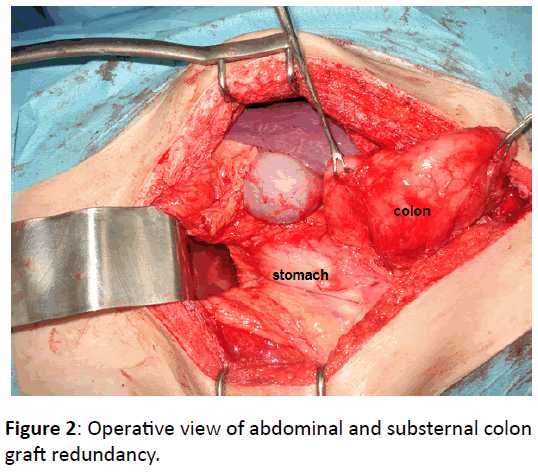
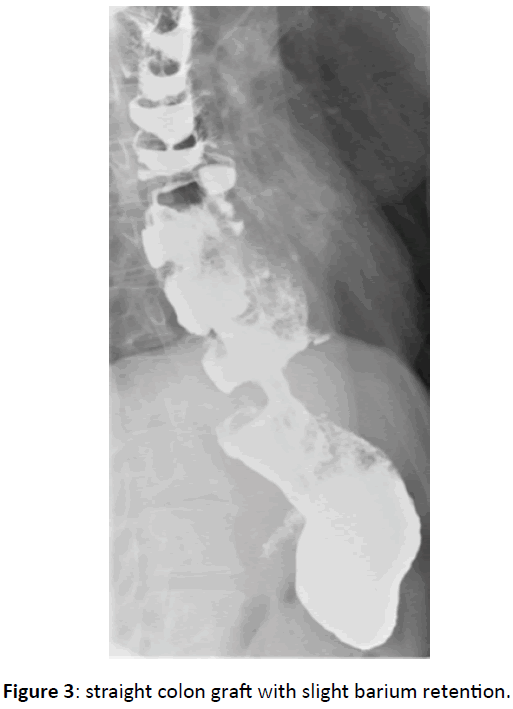
A 24 –year- old woman underwent a substernal left colon interposition based on left colic vessels for esophageal caustic stricture. The functional results were good with improvement in nutritional status and life quality. Seven years after esophageal reconstructive surgery, patient started to develop progressive dysphagia, nocturnal regurgitation, and intermittent episodes of vomiting and cervical postprandial swelling. After life-style modifications and medical treatment, a slightly symptomatic improvement was noted. After a short period, the patient reported an aggravation of her symptoms which became disabling with negative impact on her socioprofessional life. She was investigated with a liquid barium study (Figure 1) which demonstrated a hold up of contrast product above the substernal hiatus with dilation loop of retrosternal colon graft, the inta-abdominal part of colon was not dilated. A computed tomography (CT) scan performed confirmed the colon dilation with tortuous aspect of retrosternal colon graft segment. Despite the life-style modification measures, short-term evolution was marked by aggravation of symptoms with nutritional disorders and important negative impact on work-life. +++A surgical correction was indicated and through sterno-laparotomy, the retrosternal redundant colon segment was completely mobilized with taking care to preserving intact the main vascular supplying pedicle of graft (Figure 2). The cause of redundancy was the adhesions at the retrosternal hiatus associated with angulation of graft when leaving substernal space and passing into the abdominal cavity. The redundant part of colon was resected and colocolic re-anastomosis in end-to-end fashion was performed. The adhesions were corrected, retrosternal hiatus was enlarged and colon was straightened (Figure 2). The patient had uneventful recovery. Oral intake was resumed on day 7 and patient discharged on 14th postoperative day with normal diet and complete symptomatic improvement. Oral contrast study performed 36 months later revealed a straightened colon graft with good clearance of contrast meal (Figure 3).
Case 2
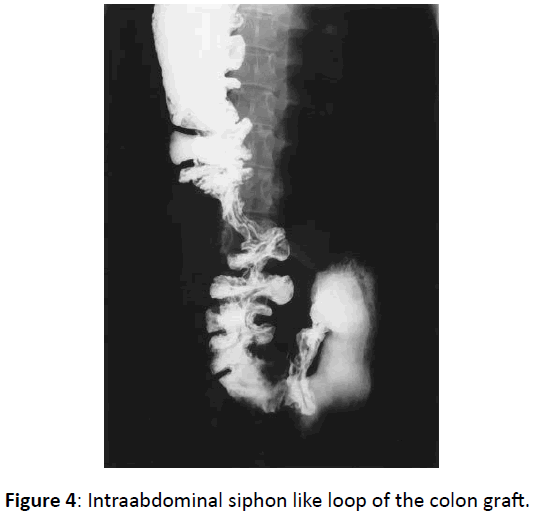
A 26-year-old man who underwent colon interposition with intrathoracic anastomosis for esophageal caustic stricture. Five years after initial surgery, the patient developed progressively dysphagia, intractable regurgitation, and sensation of fullness in the chest, intermittent late postprandial vomiting and occasional episodes of pneumonia. Investigations were performed including a barium swallow study showed a siphon like appearance of the distal segment of the transposed colon (Figure 4), despite a significant increase in the transit time throughout the colon graft, the gastric emptying was normal. Upper gastrointestinal endoscopic examination demonstrated a patent esophagocolic anastomosis situated at 25 cm from the incisors, and a marked tortuosity of the intraabdominal part of the colon graft. The loop was about 13 cm in length and the cologastric anastomosis was slightly strictured CT scan revealed dilation of colon graft part situated immediately prior to cologastric anastomosis. After failure of life-style modifications measures and aggravation of clinical symptoms, it was decided to attempt surgical correction of redundant colon segment +++.
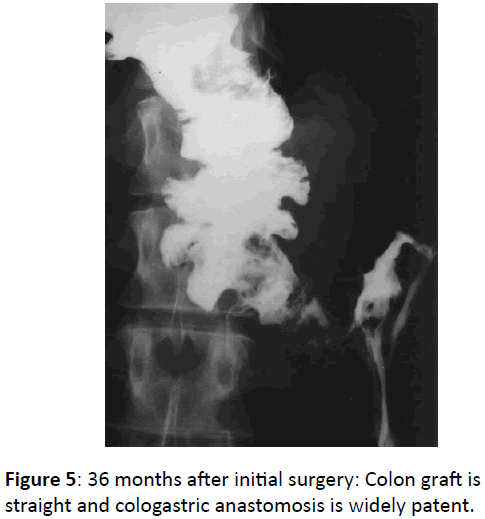
Through an iterative abdominal incision, the redundant graft segment was mobilized carefully and care was taken to avoid injury to its supplying vascular pedicle. There were no hiatal adhesions causing mechanical obstruction. Dissection was continued and cologastric anastomosis was identified. After hand- exploration, the anastomosis between the colon graft and posterior side of stomach was partially structured. Approximately 15 cm of distal redundant colon was resected without causing injury to the main vascular pedicle supplying the colon graft. A new end–to-end cologastric anastomosis was performed with interrupted suture. The early postoperative outcome was uneventful and patient resumed oral intake with immediate improvement in her preoperative symptoms. The patient was discharged on day 14 with ability to eat a normal diet. A barium study performed 6 months after surgery, demonstrated a straightened colonic graft with minimal hold up (Figure 5).
Discussion
Both left and right colon can be used as esophageal substitute to replace diseased esophagus. Successful esophageal reconstruction by colon interposition includes: selection of colon segment which has less variation of blood supply, using a colon graft with adequate length avoiding excess, When the graft is pulled up to the neck through substernal or mediastinal route, it is primordial to make interposed graft straight avoiding kinking and twist of graft and to eliminate any obstructive elements at the substernal and esophageal hiatus, and at the thoracic inlet. The need for reoperation after esophageal reconstruction with colon interposition ranges from 15% to 30% in the reported several series [1,2]. Redundancy of the interposed colon is a late mechanical complication and can occur several decades after initial reconstructive surgery [1]. The incidence of colon redundancy appears to augment with the duration of follow up and it varied between 8 and 21% [7-10]. This reported incidence is probably underestimated because many patients may adjust their life-style or make dietary modifications without ever seeking medical assistance and do not report occasional symptoms such as regurgitation or aspiration signs. Re-surgery was frequently performed for colon redundancy and surgical correction is required in 8–22% of patients after long-term follow up [7,11-14]. Redundancy of colon graft leads to food and liquid retention in the redundant graft, regurgitation, and an increased risk of nocturnal aspiration. Clinical symptoms of redundancy includes dysphagia, retrosternal fullness, regurgitation, chest pain, aspiration pneumonia and cervical bulging [15,16]. The intensity of symptomatology is correlated to the importance of colon dilation. In order to facilitate emptying of the colon graft, some patients preferred sleeping in the prone position. These classical symptoms with varying intensity were seen in the two patients of our study. Surgical correction was indicated in both patients to prevent potentially debilitating nutritional and pulmonary complications and to improve quality of life. The nutritional status of patient was evaluated on the basis of weight loss and serum albumin rate. Improvement of patient nutritional status before surgery is highly recommended to decrease risk of anastomotic complications. Both parenteral and enteral nutrition were used to correct nutritional disorders of these two patients before time of surgical correction. As suggested by authors, the excess length of colon graft favors the development of interposed graft redundancy. [2,10,15,16]. The length of the colon graft is usually significantly greater than the length of its vascular pedicle which conditions the graft ascension to the neck. While the vascular supply usually adopts a straight line in its course from the abdomen to the cervical region, the colon itself can easily adopt a tortuous course due to its excessive length. It is so important to use a colon graft with adequate length to ensure a tension-free anastomosis and to avoid excess. [10,16]. As being a thinwalled pliable hollow organ, the colon responds to the negative intrathoracic pressure by passively dilating over time above any point of partial obstruction, such as the narrowed thoracic inlet, the aortic arch, a narrowed hiatus at the diaphragm, or a strictured cologastric anastomosis [15]. Mechanical obstruction at the retrosternal hiatus also may be responsible for proximal dilatation and redundancy of a retrosternal colon graft. It is therefore primordial and important to remove any potential obstructing elements during the initial surgical procedure of reconstruction. Examples include the opening of the thoracic inlet by removing manubrium and head of the left clavicle, widening the diaphragmatic hiatus and performing a wide, well vascularized cologastric anastomosis. In order to ensuring maintaining the cologastric anastomosis located intra-abdominally, the colon graft should be fixed on its antimesenteric border to the diaphragmatic wall to avoid intrathoracic ascension of the cologastric anastomosis [8,9]. The point of obstruction in patient 1 was to be adhesions at the retrosternal hiatus and acute angulation of graft created when it left the substernal space and passed intraabdominally. While in patient 2 the cause appeared to be the cologastric anastomosis stricture. Functional results and life quality of patients underwent colon interposition can be affected by the occurrence of interposed graft colon redundancy. This mechanical disorder of graft occurs during long-term outcomes after initial reconstructive surgery. Over the years, food retention in redundant colon aggravates the colon graft dilatation leading to debilitating symptoms and nutritional disorders. In such situation, investigations are very useful to diagnose redundancy, evaluate its gravity and to plan the appropriate surgical treatment. A barium swallow and meal are useful to provide information about the anatomical arrangement of the interposed colon and to accurately identify the redundancy area. Endoscopy and CT scan of the neck, chest and abdomen can be of considerable contribution to more accurate the diagnosis. Several surgical options have been proposed to correct redundancy of interposed colon graft. The surgical approach is dictated by the anatomical site of redundancy and the initial route of reconstruction. Laparotomy combined with a median sternotomy, thoracotomy with or without laparotomy, or thoraco-laparotomy can be employed to easily access to the redundant segment of colon graft. Straightening and anchoring the redundant colon part without reducing its length and its diameter is usually unsuccessful in the long term in improving symptoms [17]. Resection of redundant part of colon graft with either re-anastomosis or coloplasty and sideto- side bypass of redundant colon area are the reported techniques used frequently to surgically manage colon graft redundancy [17-19]. Narrowing colon lumen by resecting the colon antimesenteric border with a linear stapling device may be necessary when the redundant colon shows gross dilatation. Any obstructing elements or adhesions should be corrected. When dissecting colon graft, precautions must be taken to prevent injuring or compromising the vascular pedicle supplying colon graft. Therefore any dissection should take place close to the wall of the colon, dividing only terminal vessels supplying the part of colon to be resected [17-19]. In particular situation when iterative surgeries performed to correct colon graft redundancy fail, new esophageal reconstruction using sufficient remnant stomach or colon can be proposed as a surgical alternative option for treatment. So redundancy of colon graft is the main late mechanical complication of colon interposition following esophagectomy. The interposed colon graft acts mainly as passive conduit and the food bolus travels mainly through the colic transplant by gravity. Proper attention to the length of the colon segment intraoperatively and relieving any obstructing elements are important paramounts to minimize the risk to develop this long-term mechanical disorder of colon graft. Therefore making graft straight, using a graft with adequate length or excising the excess part of conduit, eliminating any obstructing elements such as enlarging thoracic inlet, retrosternal hiatus and esophageal hiatus and at last performing a large cologastric anastomosis to facilitate graft emptying ant to prevent anastomotic stricture.
Conclusion
Colon graft redundancy is the most common long-term mechanical complication occurred following colon interposition for esophageal reconstruction. After preoperative accuracy of the identification of the redundant colon part, surgery is indicated to relieve debilitating symptoms and improve the patient’s quality of life.
Conflict of Interests
The authors declare that they do not have conflict of interests.
References
- Shokrollahi K, Barham P, Blazeby JM, Derek A (2002) Surgical revision of dysfunctional colonic interposition after esophagoplasty. Ann Thorac Surg 74: 1708-1711.
- Peters JH, Kauer WK, Crookes PF (1995) Esophageal resection with colon interposition for end-stage achalasia. Arch Surg 130: 632–637.
- Cerfolio R J, Allen MS, Deschamps C, Trastek VF, Pairolero P C (1995) Esophageal replacement by colon interposition. Ann Thorac Surg 59: 1382–1384.
- Curet-Scott MJ, Ferguson MK, Little AG, Skinner DB (1987) Colon interposition for benign esophageal disease. Surgery 102: 568–574.
- Clark J, Moraldi A, Moossa A R, Hall A W, DeMeester TR, et al. (1976) Functional evaluation of the interposed colon as an esophageal substitute. Ann Surg 183: 93–100.
- Wain J C, Wright C D, Kuo E Y (1999) Long-segment colon interposition for acquired esophageal disease. Ann Thorac Surg 67: 313–317.
- Ahmed A, Spitz L (1986) The outcome of colonic replacement of the esophagus in children. Prog Pediatr Surg 19: 37–54.
- DeMeester T R, Johansson K E, Franze I (1988) Indications, surgical technique, and long-term functional results of colon interposition or bypass. Ann Surg 208: 460–474.
- DeMeester S R (2001) Colon interposition following esophagectomy. Dis Esophagus 14: 169–172.
- Abdelkader Boukerrouche (2016) 15-year Personal Experience of Esophageal Reconstruction by Left Colic Artery-dependent Colic Graft for Caustic Stricture: Surgical Technique and Postoperative Results. J GHR 5: 1931-1937.
- Kelly J P, Shackelfor G D, Roper C L (1983) Esophageal replacement with colon in children: functional results and long-term growth. Ann Thorac Surg 36: 634–643.
- Mutaf O, Ozok G, Avanoglu A (1995) Oesophagoplasty in the treatment of caustic oesophageal strictures in children. Br J Surg 82: 644–646.
- Bonavina L, Chella B, Segalin A, Luzzani S (1998) Surgical treatment of the redundant interposed colon after retrosternal esophagoplasty. Ann Thorac Surg 65: 1446–1448.
- Abdelkader Boukerrouche (2014) Isoperistaltic left colic graft interposition via a retrosternal approach for esophageal reconstruction in patients with a caustic stricture: mortality, morbidity, and functional results. Surg Today 44: 827-833.
- Jeyasingham K, Lerut T, Belsey R H (1999) Functional and mechanical sequelae of colon interposition for benign oesophageal disease. Eur J Cardiothorac Surg 15: 327–331.
- Domreis J S, Jobe B A, Aye R W, Deveney K E, Sheppard B C, et al. (2002) Management of long-term failure after colon interposition for benign disease. Am J Surg 183: 544–546.
- Schein M, Conlan A A, Hatchuel M D (1990) Surgical management of the redundant transposed colon. Am J Surg 160: 529–530.
- Shokrollahi K, Barham P, Blazeby J M, Alderson D (2002) Surgical revision of dysfunctional colonic interposition after esophagoplasty. Ann Thorac Surg 74: 1708–1711.
- Urschel J D (1996) Late dysphagia after presternal colon interposition. Dysphagia 11: 75–77.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences